Shoulder Pain and the Potential Role of Acupuncture: A Narrative Review of Clinical Practice and Treatment Guidelines
Article information
Abstract
The potential use of acupuncture for shoulder pain of various etiologies and whether clinicians make recommendations about the use of acupuncture was examined. Shoulder pain is a common clinical problem. What is the level of evidence and how often is acupuncture recommended for shoulder pain? A manual and database (PubMed) search of review articles of related clinical trials and guidelines was performed. The evidence for effectiveness of acupuncture treatment of different types of shoulder pain was weak. However, there are some studies, with a weak to moderate level of evidence, on shoulder pain (across nine subtypes of shoulder pain). Acupuncture is safe and may be a cost-effective treatment for shoulder pain. There were 131 statements recommending the use of acupuncture for shoulder pain across 12 subtypes of shoulder pain. The most common statements were for non-specific ‘shoulder pain.’ There were 11 statements against the use of acupuncture for shoulder pain and three subtypes of shoulder pain. The level of evidence in studies of acupuncture treatment for shoulder pain is low, therefore, further research is needed. Recommendations for the use of acupuncture for shoulder pain are increasing but lag behind those for other pain problems such as low back pain.
Introduction
Shoulder pain is a relatively common problem that patients present with in clinical practice [1]. While estimates of the number of cases of shoulder pain vary considerably [2], few studies examining the prevalence have been conducted [3]. Shoulder pain has been reported to be the third most common musculoskeletal problem in general practice and it accounts for around 1% of all consultations [1,4,5]. Of the consultations for musculoskeletal pain, 16% are for shoulder pain [1,6]. The cumulative incidence in the age group 45–64 was 2.4% [3], and a lifetime prevalence was estimated as 70% [5]. Furthermore, females and the elderly are at higher risk of shoulder pain [1,2,4,6].
Shoulder pain can develop following injury or stroke but it more commonly occurs during daily activities such as athletic injuries, machine handling, and overhead lifting. In general practice, the four most common causes of shoulder pain are rotator cuff disorders (including injuries, and bursitis), glenohumeral disorders (including adhesive capsulitis and arthritis), acromioclavicular joint disease (including injuries, and osteoarthritis), and pain referred from the neck [1,5,7]. Other forms of shoulder pain include intrinsic or extrinsic instability, cancer pain [7], and post-stroke pain [8].
Once the case has been triaged, early treatment commonly includes referral for physiotherapy [9]. Surgery is an option for some shoulder problems, but is usually only offered when conservative treatments have been tried and failed [1]. As with other pain problems, active treatments such as exercise are encouraged, but pain control is necessary. Inadequate pain management reduces compliance with the active treatments [10]. Exercise and stretching are recommended but it has been reported that the evidence for them is not strong, and usually exercise and stretching comes with the recommendation to use over the counter analgesics [1,4]. Other therapies such as acupuncture have been recommended because, “Acupuncture can reduce pain, allowing the patient to participate in exercise therapy” [10].
The recent clinical practice guideline (CPG) from the UK National Institute of Health and Care Excellence (NICE) for chronic pain reported that most forms of pharmacological intervention were not very effective and/or have significant adverse effect profiles [11], thus, only anti-depressant medications are now recommended, and non-pharmacological therapies such as exercise, cognitive behavioral therapy, and acupuncture are the primary treatments recommended for chronic pain in patients who are 16 years and older [11]. Furthermore, acupuncture may be helpful for more acute pain conditions including postoperative pain [12]. Acupuncture is also recommended for treatment of acute pain in adults [13] and children in Australia [14]. The New Zealand Government group, the Accident Compensation Corporation, recommended acupuncture for adhesive capsulitis as early as 2004 [15] despite the paucity of evidence for acupuncture in shoulder pain [16].
What is the evidence for efficacy in acupuncture treatment for shoulder pain and how often have experts applied that evidence and made recommendations about acupuncture for shoulder pain? This brief narrative review will present an overview of current evidence for acupuncture in the treatment of shoulder pain, and a summary of current findings regarding recommendations for or against the use of acupuncture in the treatment of shoulder pain.
Recommendations are made in two forms of publication. The first, the CPG is a formal document that follows scientifically established rules for collecting, evaluating, and judging evidence for therapies for a particular condition. CPGs also tend to be more technical and published in specialized websites or medical journals. Treatment guidelines (TGs) are less formal publications aimed at increasing accessibility to patients. They are less technical, simpler, and written using lay language [17]. The primary purpose of the TG is to inform the patient (with minimal inclusion of technical evidence or terminology) for the purposes of increasing implementation of treatment recommendations.
Materials and Methods
The search for review articles of acupuncture treatment of shoulder pain was conducted manually and electronically (PubMed on April 22, 2022) using the terms ‘shoulder pain,’ ‘acupuncture’ and ‘review.’ Reviews of shoulder pain conditions and levels of evidence for each are summarized narratively. The first author has been searching for CPGs and TGs since 2013, building a data base of these publications. The search methods are described elsewhere [17] and elaborated in the supplemntary file.
Several articles have been published from this data base presenting overviews of findings for the recommendation of use for acupuncture in general [17], back pain [18], overall health [19], oncology [20], palliative care [21], chronic pain [22], and post-stroke care [23]. The library created had more than 3,500 publications making almost 9,000 recommendations, covering over 500 different symptoms including shoulder pain, adhesive capsulitis, rotator cuff injury, and impingement syndrome.
Results
1. Clinical evidence
Some reviews have reported that studies on acupuncture for shoulder pain have provided a very low level of evidence [24–26] for adhesive capsulitis [27,28], rotator cuff disorder [24,29], shoulder pain [30,31], subacromial pain [32], and subacromial impingement syndrome [28,33]. Other reviews have reported a low level of evidence across a range of shoulder pain conditions. In some reviews acupuncture has been reported to be effective compared with sham acupuncture for shoulder pain [34–36]. In other reviews, acupuncture has been reported to be effective for shoulder pain [28,34–40], shoulder-hand syndrome [41,43], shoulder impingement syndrome [39,44,45], rotator-cuff pathology [46], shoulder injuries [39,47], subacromial shoulder pain [48,49], adhesive capsulitis [46,50–52], pain of humeral fractures [53], post-stroke shoulder pain [8,39,54], and post-stroke shoulder-hand syndrome [55]. A review by MacPherson et al reported that the effects of acupuncture including sham acupuncture-controlled trials persisted up to one year after treatment [56].
2. Safety and cost-effectiveness
Over the decades, acupuncture has been described as a safe therapy when in the hands of qualified practitioners [16,46,57–63]. While the literature search did not retrieve specific studies on the cost-effectiveness of acupuncture in shoulder pain, one study of dry needling reported the cost-effectiveness of treatment (for subacromial pain syndrome) [64]. However, the findings of cost-effectiveness for acupuncture treatment for pain in the neck, back, knee (OA pain), and head [65,66] may imply that acupuncture treatment for chronic shoulder pain could be cost effective, but this needs to be studied. For a therapy to be considered for inclusion in CPGs/TGs, a therapy is required to be safe, show evidence of effectiveness, and cost-effectiveness [17].
3. Recommendations
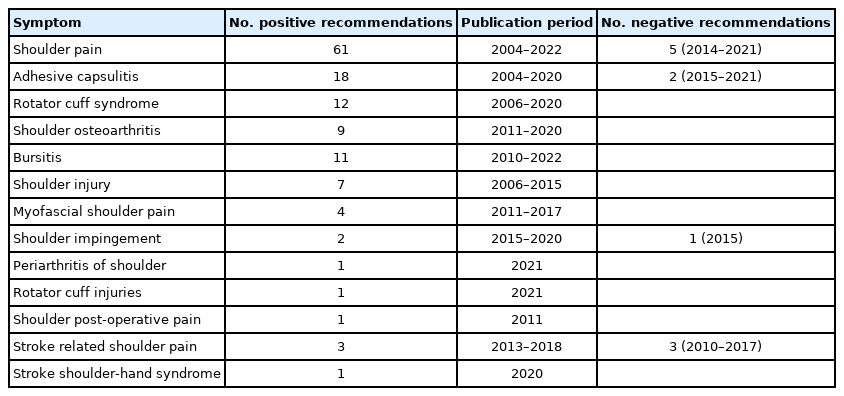
Many groups have recommended the use of acupuncture as an adjunctive treatment to help with shoulder pain. The number of times acupuncture was recommended for each type of pain problem, and the range of years in which these recommendations were made are listed in Table 1. Only publications that specified the shoulder or shoulder structures were included, thus publications recommending acupuncture for conditions such as ‘joint pain,’ ‘arthritis pain,’ ‘osteoarthritis pain,’ ‘rheumatic pain,’ ‘rheumatoid arthritis,’ ‘chronic pain,’ ‘acute pain,’ neck pain,’ ‘pain management,’ ‘stroke rehab,’ have not been included. Several groups have recommended against the use of acupuncture due to inadequate studies or a weak level of evidence for shoulder pain (5 negative recommendations), adhesive capsulitis (2 negative recommendations), rotator cuff impingement (1 negative recommendation) and stroke related shoulder pain (3 negative recommendations; Table 1). Four of the recommendations against acupuncture for shoulder pain came from the US insurance company AETNA, which updates its statements about acupuncture regularly [67]. The number of positive recommendations over time are shown in Table 2. CPGs and TGs have made recommendations for the use of acupuncture as a treatment option for various forms of shoulder pain (Table 3) [68–74].
Discussion
This review reports relatively weak, but emergent positive evidence that acupuncture may be effective for shoulder pain resulting from a variety of causes. Safety, efficacy, and cost-effectiveness of acupuncture allows guideline development groups to examine the potential use of acupuncture for the treatment of shoulder pain. The literature search in this review revealed 131 CPGs and TGs recommendations to use acupuncture for shoulder pain (in general and 12 subtypes of shoulder pain). There were 11 recommendations against the use of acupuncture for shoulder pain (in general and three subtypes of shoulder pain). Recommendations for acupuncture treatment of nonspecific ‘shoulder pain’ were the most common, and most recommendations were TGs rather than CPGs, of which most came from the UK, USA, Australia, and New Zealand.
Recommendations to use acupuncture for shoulder pain have increased over time and appear to follow evidence-based publications. The Cochrane review of acupuncture for shoulder pain in 2005 drew the first tentative positive conclusions for the use of acupuncture [37]. Since then, there has been an increase in the number of publications (2008–2011; Table 2). The next major publication on the use acupuncture for shoulder pain, was a high-quality meta-analysis with large sample sizes based on individual patient data (which is considered the gold-standard of evidence synthesis), drew positive conclusions about the use of acupuncture in chronic shoulder pain in 2012 [34], and is followed by a clear increase in the number of publications recommending acupuncture seen in the years between 2014–2021 (Table 2). To provide a more precise answer about the relationship between evidence and recommendations, a more formal study exploring the quality of CPGs on acupuncture for shoulder pain, and the degree to which they follow the emerging evidence is needed. This remains a problem in general CPG development [75] but may be better addressed in guidelines that recommend acupuncture [76]. As discussed above, NICE determined that the treatment of chronic pain conditions with pharmacological treatments was ineffective and led to the removal of almost all the usual medicinal drugs. Acupuncture is now recommended by NICE as a primary treatment for chronic pain, despite moderate to weak evidence, acupuncture treatment of chronic pain has a good safety record [11]. Clinicians that develop treatment guidelines weigh the benefits and risks of each therapy and compare treatments with each other, which allows recommendations to be made for a therapy, even when its evidence is not strong. Compared with back pain, the evidence for acupuncture treatment of shoulder pain is not as strong and is not as consistent, hence we see less CPGs for acupuncture treatment of shoulder pain than we do for back pain [18]. For example, NICE recommends acupuncture for non-specific chronic back pain and headaches [11,77], as does the German CPG publication group the Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften e.V. (AWMF) [78,79]. However, neither group recommend acupuncture for shoulder pain of any etiology, presumably because of the paucity of evidence. While evidence has recently emerged about the underutilization of acupuncture in guidelines and health policy due to insufficient application of the evidence for use of acupuncture [80], this current review reveals that this may not have occurred with regards recommending acupuncture for shoulder pain since the evidence is generally relatively low.
This study has several limitations. Evidence from clinical trials includes studies that did not clearly specify, identify, or separate the nature of the pathology that caused shoulder pain. Thus, there has been a tendency to generalize conditions with different and diverse pathologies. A systematic literature search of a range of electronic databases worldwide was not employed to find evidence for effectiveness of acupuncture, and important evidence may have been overlooked. However, recommendations to use acupuncture for shoulder pain are sometimes made even though the evidence is weak, so we determined that this was not a major limitation, especially considering the variability in how evidence is interpreted and used. There have been significant problems with trials that compare acupuncture to ‘sham acupuncture’ because the effectiveness of acupuncture may be underestimated and bias may be created against acupuncture [81–83]. Different review groups address evidence from sham-controlled studies in different ways.
The search performed to retrieve publications that make recommendations about acupuncture did not employ a systematic search of electronic databases and therefore may have missed publications for and against recommending acupuncture treatment for pain. The search for publications was performed primarily in English, which may have limited the search, thus, the possibility of recommendations for acupuncture treatment for shoulder pain in other languages cannot be excluded. In addition, the number of recommendations reviewed in this study included publications that update over time and republish, so may have been counted several times. It also includes publications, that are less formal than CPGs, which are relevant in informing patients about treatment options. Low adherence to recommendations in CPGs resulting from poor implementation is not uncommon [84–86]. Suggestions to improve implementation include “Development of tools to aid communication with patients” [85]. Such tools include summaries with lay language for the patient, many of these are what we have called ‘treatment guidelines,’ (TGs) [17]. While more numerous and less scientific than CPGs, TGs mostly follow the evidence, and hopefully lead to an increased implementation of related CPG recommendations. However, formal studies need to be performed to explore this.
Conclusion
The shoulder is a complex joint where many possible types and causes of shoulder pain can occur. An important component of treatment is exercise to recondition the shoulder. However, pain can limit these activities, hence, pain control is an important component of treatment. The most common approach is use of analgesic medications such as NSAIDs, though, non-pharmacological interventions for pain control are increasingly being recommended. This is because of the potential risks of medication use for chronic conditions, and because of the need to engage patients more in their own treatment process (for example engaging in therapeutic exercise). Within the range of available treatments for pain, acupuncture has emerged as a good candidate for a number of chronic pain problems, and may be a treatment option for shoulder pain.
Supplementary Materials
Supplementary material is available at doi: https://doi.org/10.56986/pim.2022.09.002.
Notes
Author Contributions
Conceptualization: SB, and MSL. Methodology: SB, MSL, TA, and THK. Formal investigation: SB. Data analysis: SB, and TA. Writing original draft: SB. Writing - review and editing: SB, MSL, TA, and THK.
Conflicts of Interest
The authors declare that they have no competing interests.
Funding
None.
Ethical Statements
This research did not involve any human or animal experiments
Data Availability
All relevant data are included in this manuscript.