Complete Remission of Drug-Induced Acute Dizziness Using Eight Constitution Acupuncture and the Barbecue Maneuver: A Case Report
Article information
Abstract
Dizziness, often symptomatic of underlying conditions, presents management challenges especially when dealing with drug-induced vestibular disorders. Complementary therapies like acupuncture, specifically, Eight Constitution Acupuncture (ECA), offers a potential alternative to other management therapies. A 74-year-old female, experiencing sudden dizziness from medication for back pain, underwent a detailed examination, constitutional diagnosis, and targeted acupuncture involving 26 insertions over 4 sessions. The treatment for dizziness, which focused on constitutional differences, integrated ECA and the barbecue maneuver which resulted in significant efficacy. A 50% reduction in the Numeric Rating Scale score from 10 to 5 was observed after the 1st session. Subsequent sessions of ECA combined with the barbecue maneuver significantly reduced symptoms of dizziness and ultimately alleviated symptoms. This case underscored the potential of ECA when combined with the application of the barbecue maneuver in treating drug-induced vestibular disorders and residual benign paroxysmal positional vertigo. The ECA’s constitutional approach allows for precise targeting and symptom resolution, and integrating the principles of Traditional Asian Medicine with biological mechanisms. Notably, this is the 1st case report of the efficacy of ECA and the barbecue maneuver in addressing drug-induced vestibular disorders. A holistic approach, considering constitutional differences, can offer insights and tailored solutions to present a promising avenue for patients experiencing such conditions. Rigorous research studies are essential to validate these findings.
Introduction
Dizziness or vertigo, although not a disease itself, often manifests as a symptom of underlying conditions, including peripheral vestibular disorders, central nervous system disorders, combined lesions, and other factors inducing dizziness or vertigo [1]. Peripheral vestibular disorders encompass conditions such as benign paroxysmal positional vertigo (BPPV), acute vestibular neuritis, Meniere’s disease, recurrent vestibulopathy, and middle ear disease [2]. The prevalence over a lifetime of moderate-to-severe symptoms from various causes of BPPV is around 30%, increasing with age, and particularly in women [3]. Dizziness or vertigo is associated with a heightened fall risk in individuals aged 65 and older [4].
Drug-induced dizziness is a complex manifestation often associated with medications such as antihypertensives and antidepressants [5]. While the prevalence of drug-induced dizziness is challenging to ascertain, management involves discontinuing the causative drug and providing symptomatic relief through pharmacological therapies such as vestibular suppressants, antiemetics, and benzodiazepines [5]. There is no clear report on the number of patients experiencing persistent dizziness, even after discontinuing medication, however, it has been reported that approximately 47% of patients who have recovered from dizziness or vertigo go on to experience recurrent episodes [6]. Pharmacological therapies often entail unavoidable side effects, necessitating complementary and alternative therapies [7].
Acupuncture, a nonpharmacological treatment, has been explored for various conditions [7–9]. The South Korean Eight Constitution Acupuncture (ECA) posits that constitutions are central determinants of physiological or pathological processes, and offers acupuncture formulas based on these constitutions [10–14]. In drug-induced dizziness, where the presumed damage is to the vestibular organ, ECA emerges as an apt method for restoring organ function. While ECA can precisely target the affected organ to provide immediate relief, there is a lack of reported cases demonstrating its immediate impact on dizziness or vertigo. This case report presents a scenario where drug-induced dizziness was entirely resolved using ECA treatment and the barbecue maneuver.
Case Presentation
A 74-year-old female experienced sudden dizziness while taking celecoxib (100 mg), acetaminophen (650 mg), eperisone hydrochloride (HCL; 50 mg), lafutidine (10 mg), and mosapride citrate dihydrate (5 mg) which were prescribed for lower back pain (left). The dizziness worsened following drug administration on the 1st day and persisted even after discontinuation (Figs. 1 and 2). The patient visited the Eight Constitution Medicine Clinic on the 4th day after symptom onset. Initially, a detailed investigation of the medications was undertaken, which determined that eperisone HCL may be the causative drug. Additionally, a pattern was observed where the dizziness worsened especially when getting up from bed or whilst turning her head left. This led us to initially suspect BPPV and/or peripheral vestibulopathy. Conditions such as vestibular neuritis and Meniere’s disease were ruled out, as there were no signs of inflammation, tinnitus, or aural fullness. Given the stable blood pressure, circulatory issues were also excluded. While central causes could not be determined (MRI scan is not available in the primary clinical setting), a physical examination revealed the absence of neurological symptoms such as diplopia, ataxia, or focal weakness. This suggested the exclusion of central vestibular disorders.
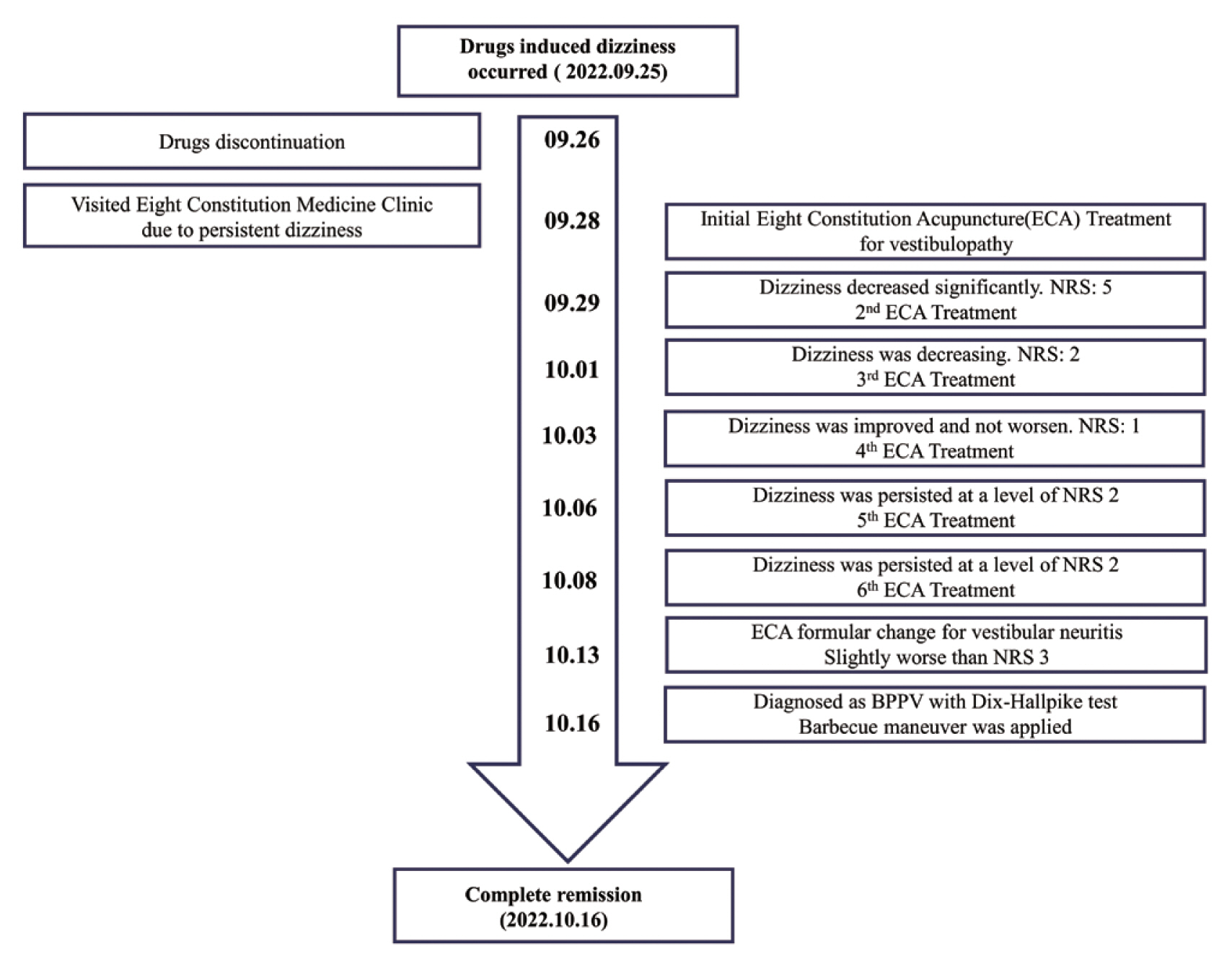
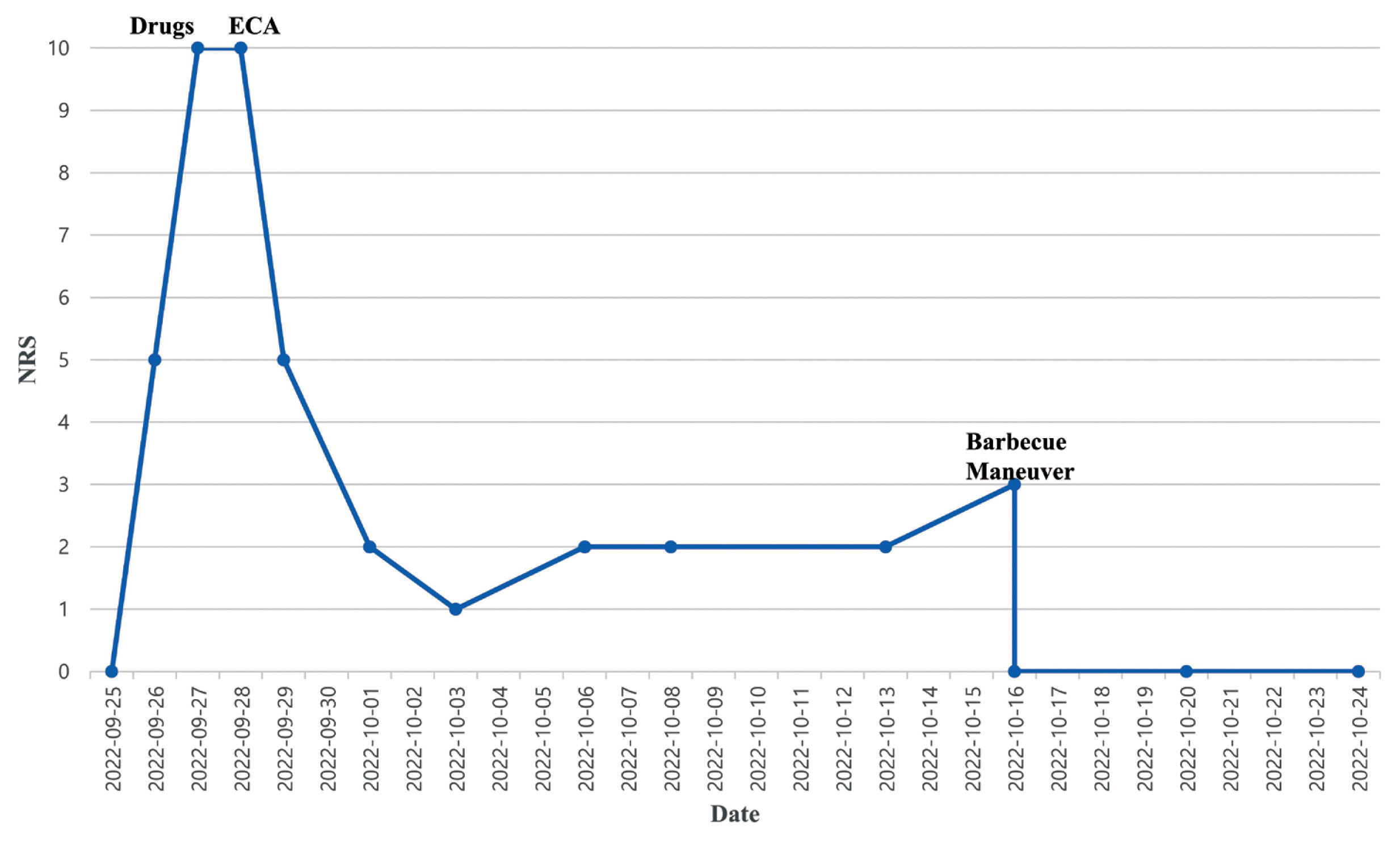
Timeline of case.
ECA = Eight Constitution Acupuncture.
NRS = numeric rating score
BBPV = Benign paroxysmal positional vertigo
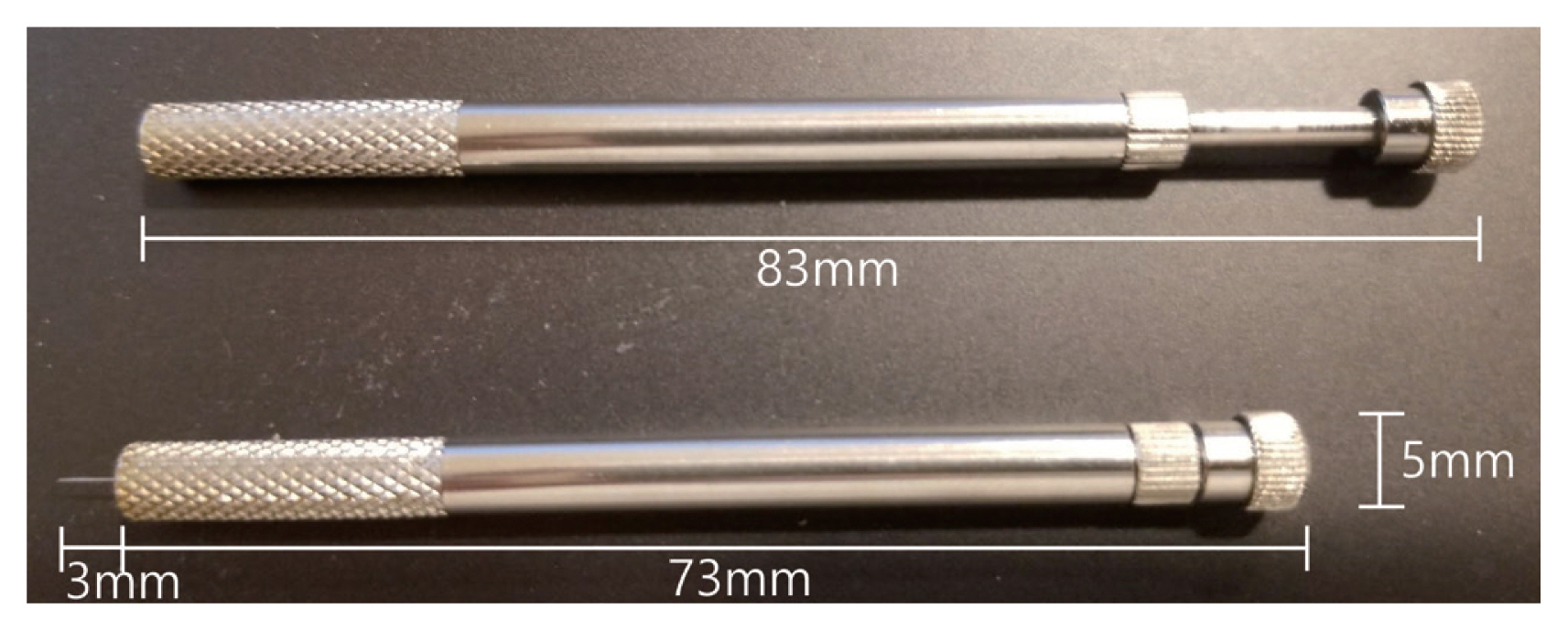
Initial ECA therapy was administered. The treatment protocol involved selecting acupuncture points based on a constitutional diagnosis through pulse examination and considering anatomical target structures. According to the constitutional acupuncture prescription, needling was determined by repeating the basic set of 4 primary acupuncture points 5 times (5 repetitions, as indicated by the symbol ‘o’ in the ECA formula), totaling 20 insertions. Of these, 2 acupuncture points are needled in the direction of meridian flow (referred to as cata-puncture), while the remaining 2 are needled in the opposite direction (referred to as ana-puncture). Additionally, 4 accessory acupuncture points, selected based on anatomical targets, were each needled once [1 time, as indicated by the period symbol (.) in the ECA formula]. To direct the meridian flow towards the upper organs, 2 out of the 4 accessory acupuncture points were needled in the opposite direction (ana-puncture) along the meridian for 2 repetitions [2 repetitions, as indicated by the comma symbol (,) in the ECA formula], resulting in a total of 6 insertions in this treatment. The entire course of treatment consisted of 26 insertions. The side of the primary treatment varied based on the constitutional type, with a focus on the left side for Vesicotonia (the name for 1 of the eight constitutions) in this case (unilateral treatment). Acupuncture points included LU8(VII′7), SP5(V′7), KI10(IX′9), SP9(V′9), LR4(I′7), and LR8(I′9). Needle techniques adhered to specific criteria such as limiting needling depth to within 3 mm of the epidermis, using the fast in fast out technique, and employing a manually administered approach [15]. A specialized acupuncture needling device was designed for use with a 0.25 mm length × 3.0 mm diameter stainless-steel needle (Fig. 3). The treatment plan comprised a total of 4 sessions, with a frequency of twice per week for 2 weeks. The barbecue maneuver was integrated into the procedure. The practitioner, a specialist in Eight Constitution Medicine, had 25 years of clinical experience and a notable patient history of over 250,000 consultations.
After receiving the 1st ECA treatment, the patient noticed a 50% reduction in dizziness, which was recorded using the numeric rating scale (NRS) to score dizziness (NRS score 10 pre-ECA pretreatment, NRS score 5 following the 1st treatment, NRS score 2 following the 2nd treatment, and NRS score 1 following the 3rd treatment; Figs. 1 and 2). Although the dizziness did not worsen, the patient desired completed symptom resolution. Therefore, the vesicotonia acupuncture formula for vestibular neuritis, with eight calculated acupuncture points, was applied (Table 1). The formula induced a slightly worse level of dizziness (NRS 3), particularly when lying on the bed or getting up and turning her neck to the left (Figs. 1 and 2). There were no other acupuncture-related adverse effects.
The Dix-Hallpike test was used to diagnose left horizontal canal BPPV, indicated by observed horizontal nystagmus on the left side. The barbecue maneuver was then applied which involved sequential rotation along the longitudinal axis of the body. During the 270-degree rotation, the process began from a supine position, turning the head toward the left side, and concluded with the nose oriented to the left, progressing in rapid 90-degree increments. Five minutes later, Dix-Hallpike testing revealed no dizziness or nystagmus in the patient’s left ear. Subsequently, all symptoms resolved (NRS 0; Figs. 1 and 2).
1. Patient perspective
Experiencing sudden dizziness, I sought help at the Eight Constitution Medicine Clinic. Despite discontinuing my medications for back pain, persistent dizziness prompted a comprehensive investigation. The ECA treatment, tailored to my constitution, involved acupuncture and the barbecue maneuver. After just 3 ECA sessions, my dizziness significantly reduced, and the subsequent use of the barbeque maneuver resolved the remaining level of dizziness. This holistic approach not only provided symptom relief but also led to a deeper understanding of the interconnected factors contributing to my vestibular concerns.
Discussion
In this case, eperisone HCL-induced acute unilateral vestibulopathy was completely resolved after applying ECA to treat vestibular system dysfunction, and the barbecue maneuver to address the remaining horizontal canal BPPV. This case report emphasizes the patient’s rapid improvement with acupuncture and manipulation, without the use of herbal medicine. Notably, this is the 1st case report of drug-induced dizziness treated with ECA and the barbecue maneuver.
Dizziness or vertigo is a symptom of central nervous system or peripheral vestibular system dysfunction and is rarely caused by ototoxic drugs such as gentamicin [3]. Among the drugs prescribed for back pain, eperisone HCL relaxes muscles, regulates blood supply to skeletal muscles, and has a few central nervous system side effects such as drowsiness [16]. It has been reported that eperisone HCL-induced dizziness is rare [17]. In this case, dizziness due to acute left vestibulopathy within the 1st 3 days of taking medication for lower back pain, raised the concern that eperisone HCL may be causing the adverse side effect. The dizziness persisted even after discontinuing the drug. Since dizziness can lead to serious problems such as falls causing fractures in older adults, prescribing and monitoring drugs with special care is necessary.
Although various pharmacological therapies are frequently used to treat acute dizziness or vertigo, unavoidable side effects often occur. Several studies have recommended acupuncture to treat acute dizziness or vertigo in cases of patients seeking emergency care or experiencing dizziness due to ischemia or cervical muscle stiffness [7–9]. However, there is no known study of acupuncture treatment for drug-induced dizziness. Simultaneously, cases attempting integrated treatment using appropriate maneuvers, as seen in this case, are novel.
Additionally, the selection of acupoints based on eight constitutions in ECA differs even for the same symptoms or diseases. The acupuncture formulae were derived from mathematical calculations based on anatomical structure and pathology [18]. In this case, Vo Ia. in the ECA formula is prescribed for treating vestibular system dysfunction in Vesicotonia. Dizziness immediately decreased from NRS 10 to NRS 5 after the first treatment session and to NRS 1 after 2 more sessions; the level of dizziness persisted for approximately 10 days. Determining the remaining drug effects was challenging 3 weeks after discontinuing the drug. We concluded that the treatment resolved the overall dysfunction of the vestibular system. However, the remaining dizziness indicated pathological conditions in other organs. Therefore, the patient was prescribed Vo IIa. of the ECA formula to normalize vestibular nerve function and the possibility of vestibular neuritis was excluded as the symptoms worsened from NRS 1 to NRS 3. The ECA formula helps to determine a prescription by accurately targeting the location of the pathology. If the exact location is not determined, the symptoms tend to increase. Therefore, ECA treatment can be used as a differential diagnostic tool.
The effectiveness of ECA in treating dizziness can be attributed to the restoration of Qi and Yin-Yang balance according to Traditional Asian Medicine meridian principles, targeting specific organ systems associated with individual constitutions. From a biological perspective, acupuncture may influence neurotransmitter release, improve blood circulation, and modulate the autonomic nervous system [7,8,19]. The integration of Traditional Asian Medicine and biological mechanisms offers a comprehensive understanding of how ECA may alleviate dizziness.
The Dix-Hallpike method determined that BPPV hypothetically caused the symptoms that persisted for approximately ten days with an NRS score of 2–3 [20]. Horizontal nystagmus confirmed horizontal canal BPPV, and the barbecue maneuver was performed [21]. The dizziness was severe on the left side; so, left rotation was performed, and the symptoms resolved immediately following the maneuver. Although ECA cures 70–80% of vestibular system dysfunction, otoconia dislodgement in the canal is a structural problem that should be addressed through appropriate maneuvers. In this case, drug-induced vestibular disorder not only impaired the function of the peripheral vestibular system but also resulted in the dislodgment of otoconia. Although the patient initially responded to ECA treatment, improving dizziness from NRS 10 to NRS 2–3, issues related to otoconia dislodgment persisted. Identifying residual symptoms linked to otoconia dislodgment through vestibular examinations determined horizontal canal BPPV. To comprehensively address this issue of dizziness, the barbecue maneuver [21], an appropriate manual technique, was employed to overcome otoconia dislodgment, resulting in complete resolution. Essentially, constitutional acupuncture restored the impaired function of the damaged vestibular system, while manual intervention effectively addressed the physical problem of otoconia dislodgment. Integrated treatment facilitated complete recovery.
The ECA is a relatively new acupuncture method initiated by its founder, Dr. Dowon Kuon, in the 1950s [18]. This approach integrates a novel application of principles from meridians, Epinger and Hess’s autonomic nervous system variability theory, and the theory of internal organ variations in traditional Korean Sasang medicine [18]. The key determinant in diagnosing the eight constitutions is the confirmation of the radial artery pulse formation on both wrists, and the distinctive feature of ECA lies in the establishment of a fundamental formula prescription composed of 4 pairs of acupuncture points [10,14,18]. The treatment is calculated mathematically based on supplementary points targeting the anatomical structures where the pathology is located. Notably, the order and frequency of needling the constituted acupuncture points must be strictly adhered to for the desired effects. The use of the “fast in fast out” needling technique is another characteristic of ECA. Importantly, the composition of acupuncture points for treatment, known as the constitutional acupuncture formula, varies significantly even for the same condition depending on the individual’s constitution. Conversely, individuals with the same constitution may receive identical prescriptions even for different illnesses.
This case report had several limitations. Firstly, it involves the observation of a single case, making it challenging to view the results as a definitive effect of acupuncture and manual therapy. Further studies are needed to confirm these findings. Secondly, the therapeutic effect in this case resulted from a combination of acupuncture and manual therapy. Consequently, the individual contributions of acupuncture and manual therapy to the treatment remain unknown. Further follow-up studies are needed to determine their respective impact. Thirdly, attempts have been made to confirm the final diagnosis through clinical reasoning. However, due to the limitations of the imaging diagnostic equipment in the primary clinic, some areas lack sufficient information to establish a definitive diagnosis. Fourthly, symptom alleviation may be related to natural recovery following drug discontinuation. However, the immediate relief of symptoms after acupuncture and symptom persistence for 3 weeks after the initial 3 sessions suggests that natural recovery is unlikely. Fifthly, vestibular organ damage was suspected to be an adverse effect of eperisone HCL; however, the effects of other drugs could not be ruled out. Therefore, future studies on the various responses of individuals to drugs according to their constitutions are necessary. Sixthly, although the effect was measured solely through the patient’s subjective NRS scores, it is necessary to objectively and systematically measure the effect using appropriate patient-reported outcome measurement tools. These limitations can be addressed through more rigorous research design in the future.
ECA may provide a new alternative for patients experiencing drug-induced dizziness. Additionally, physicians can apply appropriate maneuvers for symptoms related to structural problems, such as otoconia in the canal.
Acknowledgements
We express our gratitude to the patient for participating in this study and granting permission for the publication of this case report.
Notes
Author Contributions
Conceptualization: YC and JC. Methodology: YC. Formal investigation: YC. Data analysis: YC. Writing original draft: YC. Writing review and editing: YC and JC.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethical Statement
This case report was exempt from review by the Institutional Review Board of Sungkyunkwan University (no.: SKKU 2023-03-018). The patient provided written informed consent to participate in the study, and additional written consent was obtained for the publication of this case.
Data Availability
All pertinent data within this study and its supporting information files are available upon request.