Articles
- Page Path
- HOME > Perspect Integr Med > Volume 2(3); 2023 > Article
-
Review Article
Effectiveness and Safety of Low-Level Laser Treatment for Lumbar Disc Herniation: A Systematic Review and Meta-Analysis -
Sang Jun Lee1
 , Seung Jin Noh2,3
, Seung Jin Noh2,3 , Jeong Rock Kim2
, Jeong Rock Kim2 , Kyung Bok Park2
, Kyung Bok Park2 , Sae-rom Jeon2
, Sae-rom Jeon2 , Yejin Hong2
, Yejin Hong2 , Dongwoo Nam2,3,*
, Dongwoo Nam2,3,*
-
Perspectives on Integrative Medicine 2023;2(3):155-163.
DOI: https://doi.org/10.56986/pim.2023.10.003
Published online: October 23, 2023
1Hae Su Won Korean Medicine Clinic, Seoul, Republic of Korea
2Department of Acupuncture and Moxibustion, Korean Medicine Hospital, Kyung Hee Medical Center, Seoul, Republic of Korea
3Department of Acupuncture and Moxibustion, College of Korean Medicine, Kyung Hee University, Seoul, Republic of Korea
- *Corresponding author: Dongwoo Nam, Department of Acupuncture and Moxibustion, College of Korean Medicine, Kyung Hee University, 26 Kyungheedae-ro, Dongdaemungu, Seoul 02447, Republic of Korea, Email: hanisanam@daum.net
©2023 Jaseng Medical Foundation
This is an open access article under the CC BY-NC license (http://creativecommons.org/licenses/by-nc/4.0/).
- 1,963 Views
- 61 Download
Abstract
-
Background
- Low-level laser treatment (LLLT) is used to treat low back pain (LBP) however, its effects on lumbar disc herniation (LDH) remain unclear. The safety and effectiveness of LLLT for LDH was determined using a systematic review of randomized clinical trials.
-
Methods
- Studies on LLLT in adults with LDH were identified from 12 worldwide databases. A risk of bias assessment and a meta-analysis with categorization according to the type of control used (inactive, active, or add-on) was performed. The quality of evidence was assessed using the Grading of Recommendations, Assessment, Development, and Evaluation.
-
Results
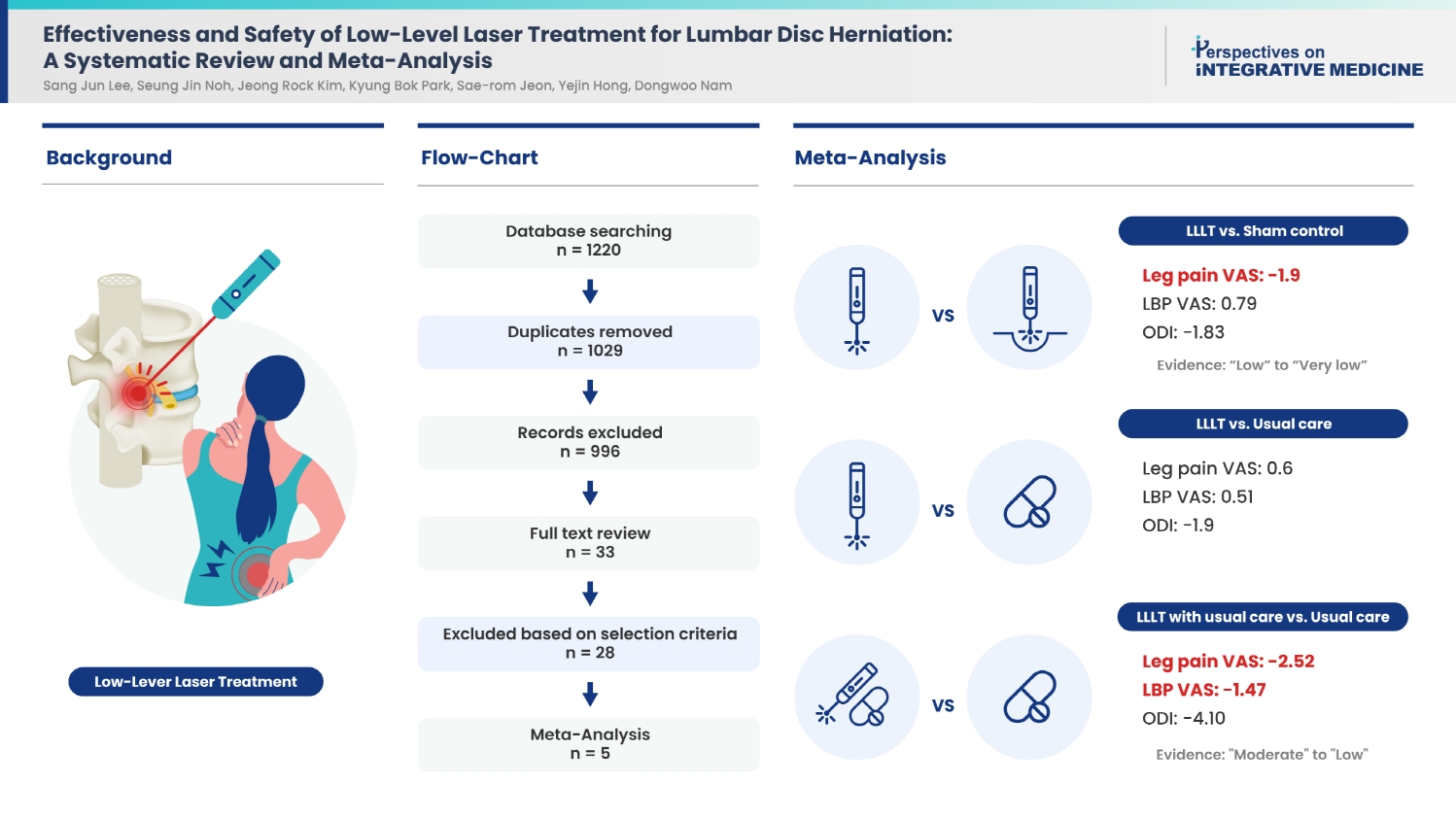
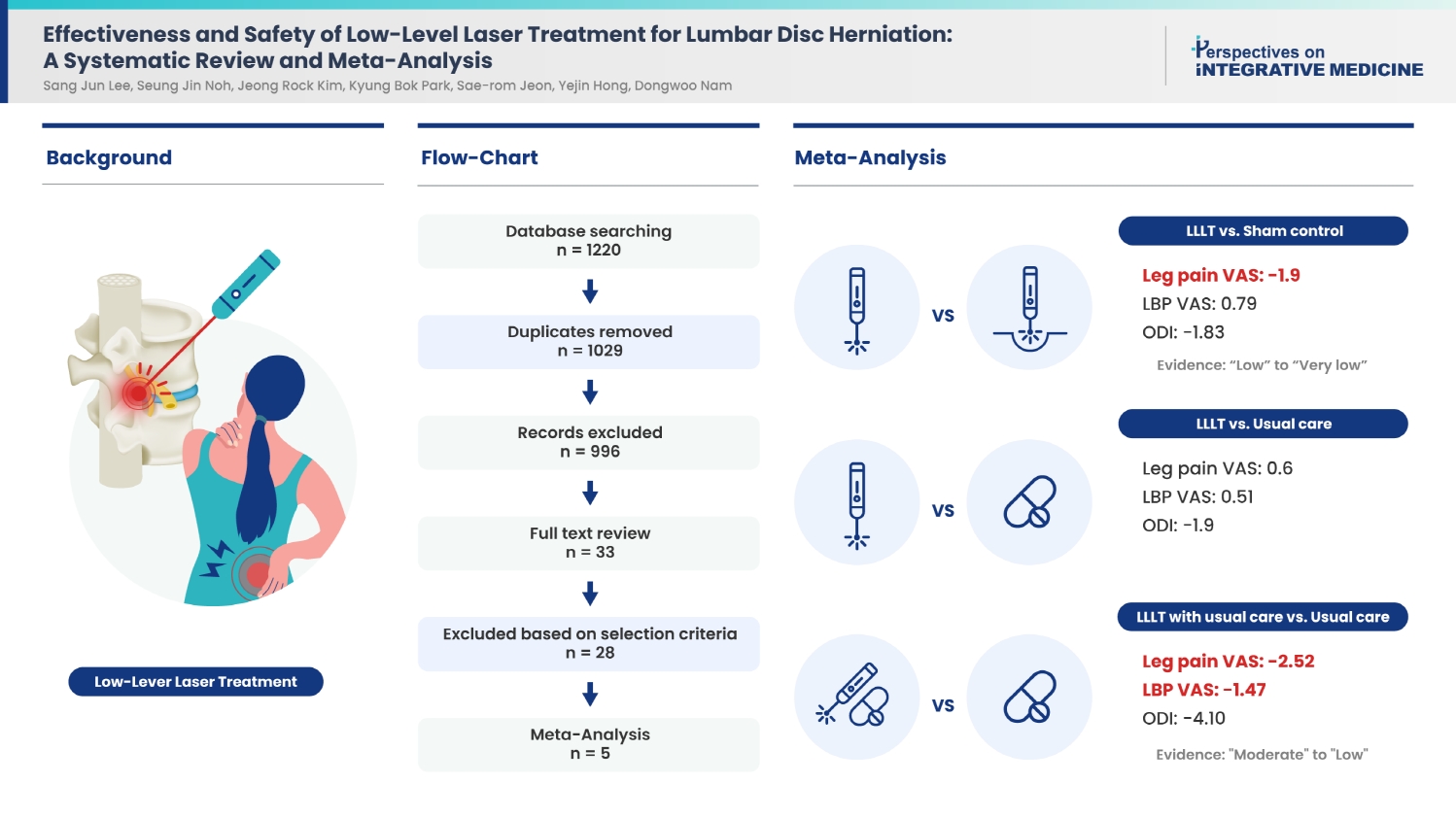
- The quantitative analyses included five studies. LLLT was significantly more effective at treating LDH [leg pain visual analog scale (VAS) mean difference (MD): −1.90, 95% confidence interval (CI): −2.01, −1.80, I2 80%; LBP VAS MD: −0.79, 95% CI: −0.87, −0.71, I2 80%] than inactive controls (placebo or sham). The quality of the evidence ranged from “low” to “very low.” As an add-on to usual care, LLLT significantly improved pain intensity and disability compared with usual care (leg pain VAS MD: −2.52, 95% CI: −2.65, −2.40, I2 97%; LBP VAS MD: −1.47, 95% CI: −1.58, −1.36; Oswestry Disability Index MD: −4.10, 95% CI: −4.55, −3.65, I2 6%). However, the quality of the evidence ranged from “moderate” to “low.”
-
Conclusion
- LLLT significantly improved outcomes compared with the inactive controls, but was not more effective than usual care for LDH. In combination with usual care, LLLT was significantly more effective than usual care alone highlighting the potential of LLLT.
- The prevalence of low back pain (LBP) and neck pain has increased substantially over the past 25 years, and in most countries, these conditions are the leading causes of years lived with disability [1]. Lumbar disc herniation (LDH), one of the most common causes of LBP and sciatica which refers to a prolapse of the nucleus pulposus, the inner core of the vertebral disc, through a tear in the outer surrounding annulus fibrosus. This results in irritation and compression of the sensory nerves, causing pain, paresthesia, tingling sensation, numbness, and muscle weakness in the distribution of the affected nerve roots [2].
- Improvements in healthcare and the advancement of medical technology have contributed to the widespread trend of population aging, resulting in a continuous increase in annual healthcare expenditure [3] owing to the increasing number of patients and medical costs related to spinal conditions/diseases. A study based on the national health insurance data of Korea, determined that the number of patients treated, and the associated medical costs for LDH increased by 1.18, and 1.53 times, respectively, over 5 years from 2006–2010 [4]. Currently, surgical and conservative treatments such as medications and physical therapy are commonly used to treat LDH [2].
- Low-level laser treatment (LLLT) is a type of phototherapy that uses low-power red and near-infrared light beams (600–1,100 nm in wavelength) for the application of light energy over the acupuncture or trigger points of affected areas, thereby affecting (stimulating or inhibiting) a wide range of cellular processes. This includes preventing apoptosis, augmenting tissue repair, and promoting tissue, and neuronal regeneration [5,6]. LLLT has been reported to reduce pain through the modulation of inflammatory processes [7]. Notably, LLLT aids in the process of photobiomodulation, affecting the biochemical processes of cells and tissues, which leads to physiological changes and promotes therapeutic effects [7]. LLLT involves no pain as it is a nonthermal process with no visible heat emission and is non-invasive. Therefore, the associated adverse events (AEs) are minimal, and serious AEs have not been reported, suggesting that LLLT may be an option for primary care [8]. Therefore, studies have been undertaken to examine the clinical efficacy of LLLT [9,10]. Currently, it is frequently used to manage symptoms in patients with musculoskeletal disorders such as myofascial pain syndrome, neck pain, nonspecific chronic LBP, and chronic joint disorders [8,10–12].
- Systematic reviews have reported on the effectiveness of LLLT for nonspecific chronic LBP [12,13]; however, there has been a paucity of reviews on LDH. Therefore, in this study, we examined the effectiveness and safety of LLLT for treating LDH through a systematic review based on randomized controlled trials (RCTs).
Introduction
- This study was based on the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement [14].
- 1. Literature search
- Three major biomedical literature databases [PubMed, the Cochrane Central Register of Controlled Trials (CENTRAL), and EMBASE] were used for the literature search. In addition, six Korean databases [KoreaMed, Korean Medical Database (KMBASE), Korean Studies Information Service System (KISS), National Digital Science Library (NDSL), https://society.kisty.re.kr from the Korea Institute of Science and Technology Information and Oriental Medicine Advanced Searching Integrated System (OASIS)], one Chinese database [Chinese National Infrastructure Structure (CNKI)], and two Japanese databases [Citation Information by NII (CiNii) and J-Stage]. The key terms used in the search included those related to symptoms of LDH (e.g., sciatica, radiculopathy), herniation of lumbar intervertebral discs (e.g., lumbar, disc), and terms related to laser treatment, including laser acupuncture (e.g., laser, LLLT, laser acupuncture), as well as a combination of these terms. The literature search was conducted on March 15, 2023. Detailed search strategies are presented in Supplementary A.
- 2. Selection of studies
- RCTs on laser therapy, including laser acupuncture for LDH, were included in the literature review. Nonrandomized controlled trials (nRCTs), uncontrolled trials such as case series, and qualitative studies were excluded. No restrictions were imposed on the language used or publication type during the literature review.
- The patient samples from this literature review included those diagnosed with LDH through radiological examination. Studies on intervertebral disc degeneration, studies in which patients with LDH were not the major participants or studies on LBP without pathoanatomical causes were excluded from the selection process.
- RCTs in which LLLT was performed for LDH were included, and studies without a clear description of the assessment of LLLT effectiveness were excluded. The selected studies were categorized into those comparing LLLT with inactive controls (placebo or sham controls), studies in which LLLT was applied as a single mode of intervention, and studies in which LLLT was applied as an add-on therapy.
- Controls and comparators in the RCTs included those with no treatment, sham LLLT, or usual care such as medication, including nonsteroidal anti-inflammatory drugs, traction, ultrasound, and exercise. In the RCTs in which other treatments were used as co-interventions in the laser treatment group, only those that received the same treatment as the co-intervention in all control or comparator groups were included in this literature review.
- 3. Data extraction
- During the study selection process, two or more independent researchers reviewed the titles and abstracts of the studies identified from the literature search to determine eligibility based on the inclusion/exclusion criteria of study selection prior to reviewing the full text of the manuscripts. When the eligibility status could not be determined based on the analysis of titles and abstracts alone, the full text of the articles was analyzed to assess eligibility. In cases where the results of the assessments conducted by independent researchers did not align, a third party was engaged to facilitate a consensus on the assessment.
- Two independent researchers analyzed the full text of the five selected studies. Data were extracted according to the established criteria of analysis for the following categories: first author, year of publication, type of study, the treatment used in the intervention group, the treatment used in the control or comparator groups, sample size, period of intervention and procedure, follow-up, outcomes measures, estimates of effectiveness, and AEs. Additionally, data on the specific methods used in the treatment, wavelength, power, energy, laser beam size, treatment time, treatment interval, and number of treatment sessions were extracted. In instances where the data extraction conducted by each researcher was inconsistent, a consensus was reached. In cases in which an agreement was not reached, a third party intervened to reach an agreement. When discrepancies arose in the results of data extraction among researchers, resolution was achieved through discussions. When the results were not in agreement, a third party was engaged to facilitate a consensus on the final data extraction.
- 4. Risk of bias
- Two independent researchers assessed the risk of bias (RoB) using the RoB tool of the Cochrane Collaboration. The seven domains of bias were: (1) random sequence generation; (2) allocation concealment; (3) blinding of participants and personnel; (4) blinding of outcome assessment (assessor); (5) incomplete outcome data; (6) selective reporting; and (7) other bias. The assessment results were categorized into three levels of RoB: high, low, and uncertain [15]. In case of disagreement in the results of the RoB assessment by the respective researchers, a consensus was achieved based on discussions between the researchers, failing which a third party was engaged to facilitate a consensus on the final assessment.
- 5. Statistical analysis
- A meta-analysis of the five selected articles was performed to quantitatively assess the effectiveness of LLLT. The results were expressed as means with standard deviations. Continuous variables were assessed using inverse variance analysis. The mean difference (MD) values were determined by comparing the intervention and control groups. The meta-analysis was performed using a fixed inverse variance method with Review Manager (RevMan) Version 5.4 (Cochrane Collaboration, 2020) software. Heterogeneity between the extracted studies was assessed using the chi-square test (are 2 variables independent of each other) and I2 (unimportant, substantial, considerable heterogeneity) statistic at a significance level of p < 0.10.
- 6. Quality of evidence
- The quality of evidence provided in the five studies included in the meta-analysis was assessed by reviewing each control and outcome variable according to the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) methodology. The quality of evidence was determined based on the GRADE criteria: RoB, publication bias, inconsistency, indirectness, imprecision, dose-response, and large magnitude of effect. The quality of each parameter was rated as “high”, “moderate”, “low”, or “very low”[16]. As only a limited number of studies were included in the analysis, publication bias was not assessed.
Materials and Methods
2.1. Study types
2.2. Participants
2.3. Type of interventions
2.4. Types of control groups
- 1. Selection of studies
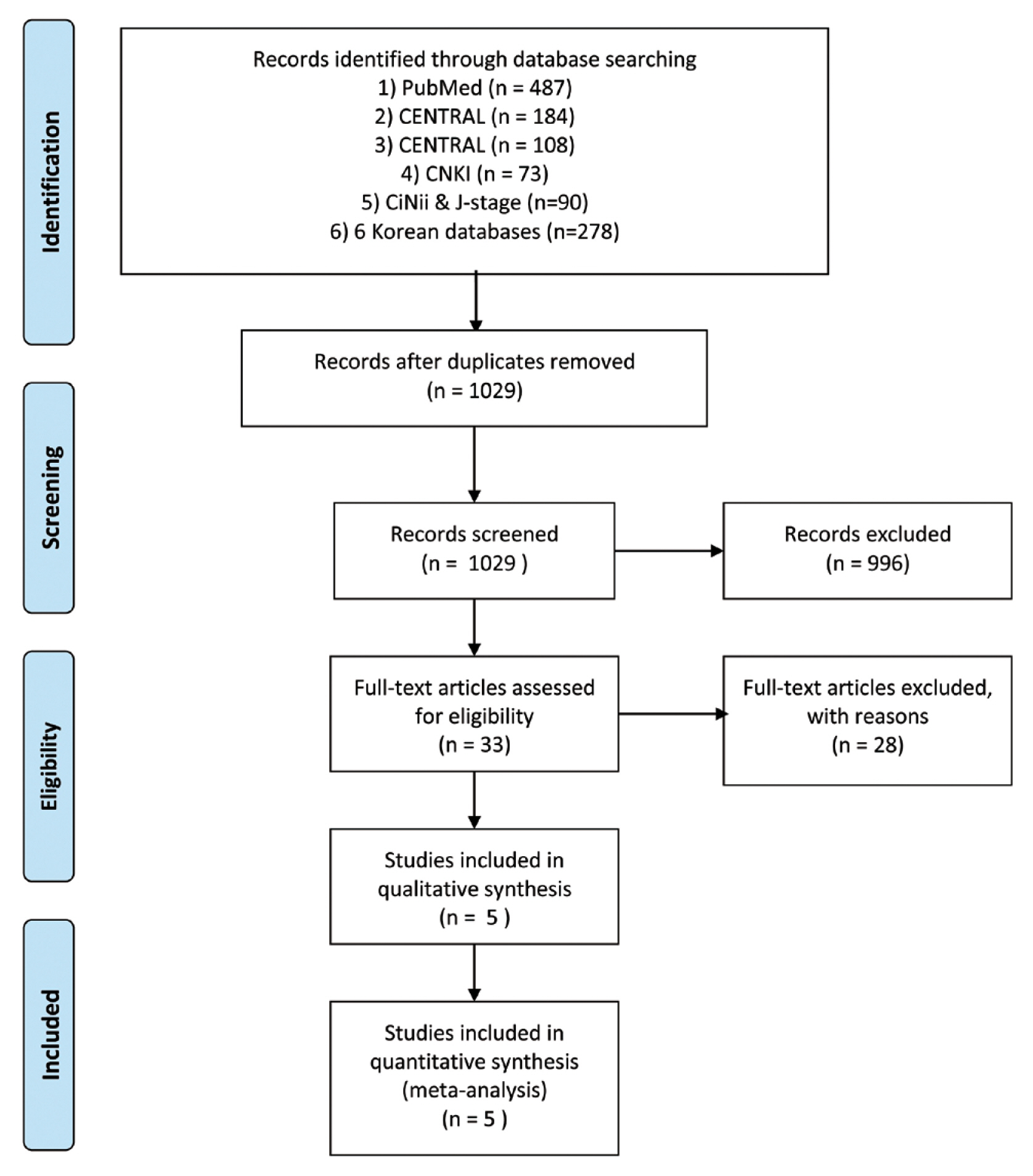
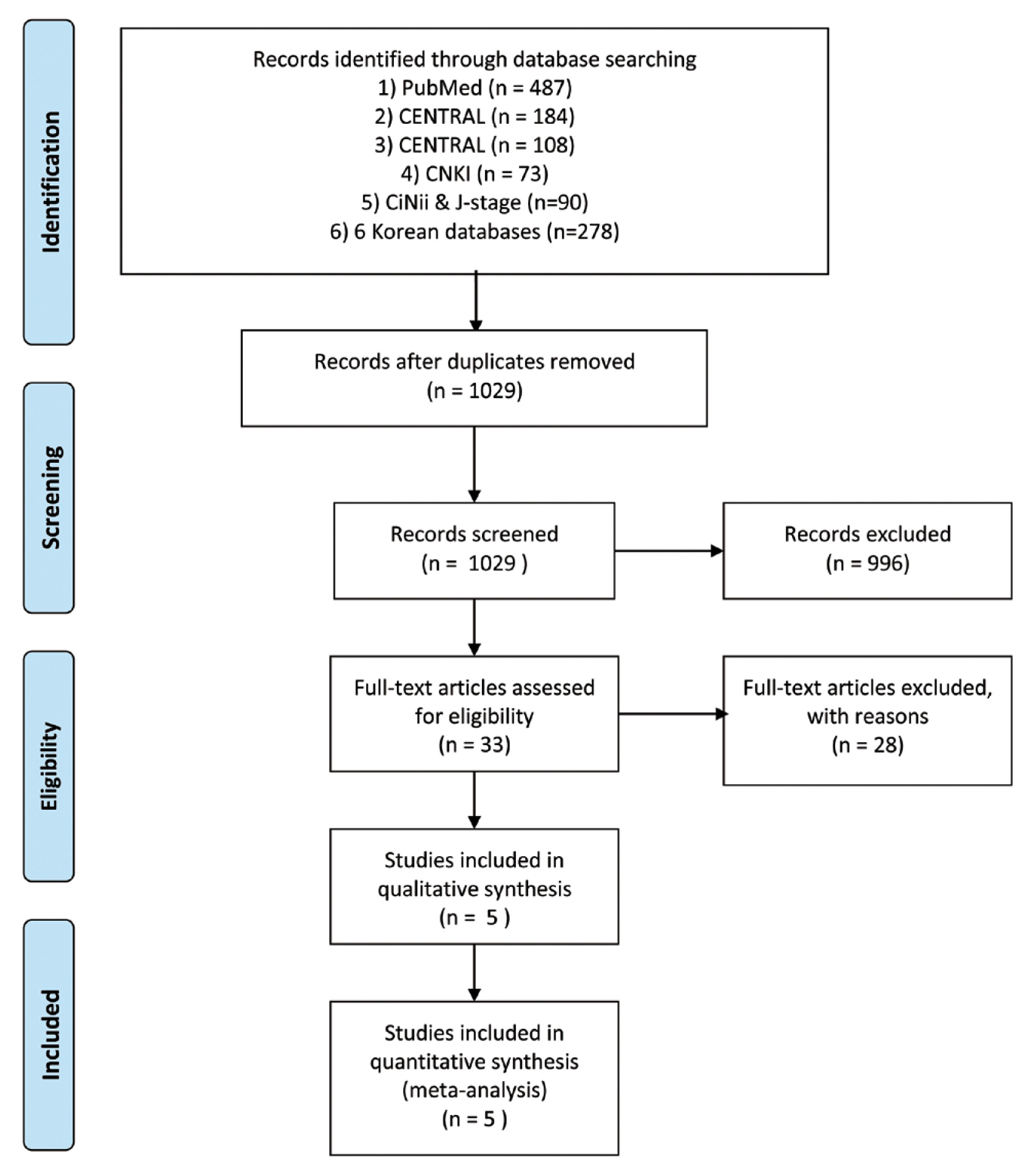
- There were 1,220 records identified, including 779 from three major biomedical databases (487 from PUBMED, 184 from CENTRAL, and 108 from EMBASE), 278 from Korean databases, 73 from Chinese databases, and 90 from Japanese databases. There were 191 duplicate records excluded, and following examination of the titles and abstracts of 1,029 articles, 996 were determined to be ineligible according to the inclusion criteria. Subsequently, the full texts of the remaining 33 studies were reviewed, and 28 studies were excluded based on the selection criteria. Consequently, the full texts of five articles were analyzed (Fig. 1).
- 2. Characteristics of studies
- From the selected five studies [17–20], 845 patients were included in this review. Of the five studies, two [17,18] were conducted in Turkey, one in Brazil [18], one in Serbia [19], and one in Pakistan [21] (Table 1 [17–21]).
- According to the inclusion/exclusion criteria for study selection, only studies on patients diagnosed with LDH based on radiological and physical examinations were included, and those on patients with LBP diagnosed with degenerative intervertebral discs were excluded. Four of the five selected studies were RCTs involving patients in an acute phase (Table 1 [17–21]).
- To assess the effectiveness of LLLT the five selected studies were categorized into three types: (1) studies comparing LLLT and sham laser treatment; (2) studies comparing LLLT with other types of usual care; and (3) studies that applied LLLT as an add-on therapy (Table 1 [17–21]). The specific treatment methods and details of the LLLT settings are summarized in Table 2 [17–21].
- Three of the selected studies [17–19] compared LLLT with sham laser treatment, and two studies [18,20] compared LLLT with types of usual care; one of the two studies [18] compared LLLT and LED treatment, and the participants performed exercises in both groups. The other two studies [19,21] were a 3-arm RCT comparing LLLT, traction, and ultrasound; thus, the effectiveness of the three different modalities was compared. Two of the selected studies [19,21] applied LLLT as an add-on therapy: one study applied LLLT in addition to the use of oral analgesics (nimesulide), and the other applied LLLT in addition to the usual care of physical therapy (Table 1 [17–21]).
- For the assessment of pain-related outcomes, the Visual Analog Scale (VAS) was used in all five studies, and most studies divided the type of pain into leg pain and LBP.
- To assess outcomes related to functional disability, the Oswestry Disability Index (ODI) and the Modified Oswestry Disability Questionnaire were used in all five studies [17–21]. Two studies also used the Ronald Morris Disability Questionnaire in their assessment [17,20].
- For mobility assessment, four studies [17,19–21] used the Schober Test and modified Schober Test to assess lumbar mobility, and the Range Of Motion was measured in four studies [17,18,20,21]. To assess the effectiveness of treatment, one study [17] used both the patient’s and physician’s global assessments. Health-related Quality of Life was assessed in one study [19], and the outcomes were presented using the Physical Component Summary and Mental Component Summary.
- Regarding other outcome measures used in the selected studies, one study [20] presented changes in the size of the herniated mass on magnetic resonance imaging.
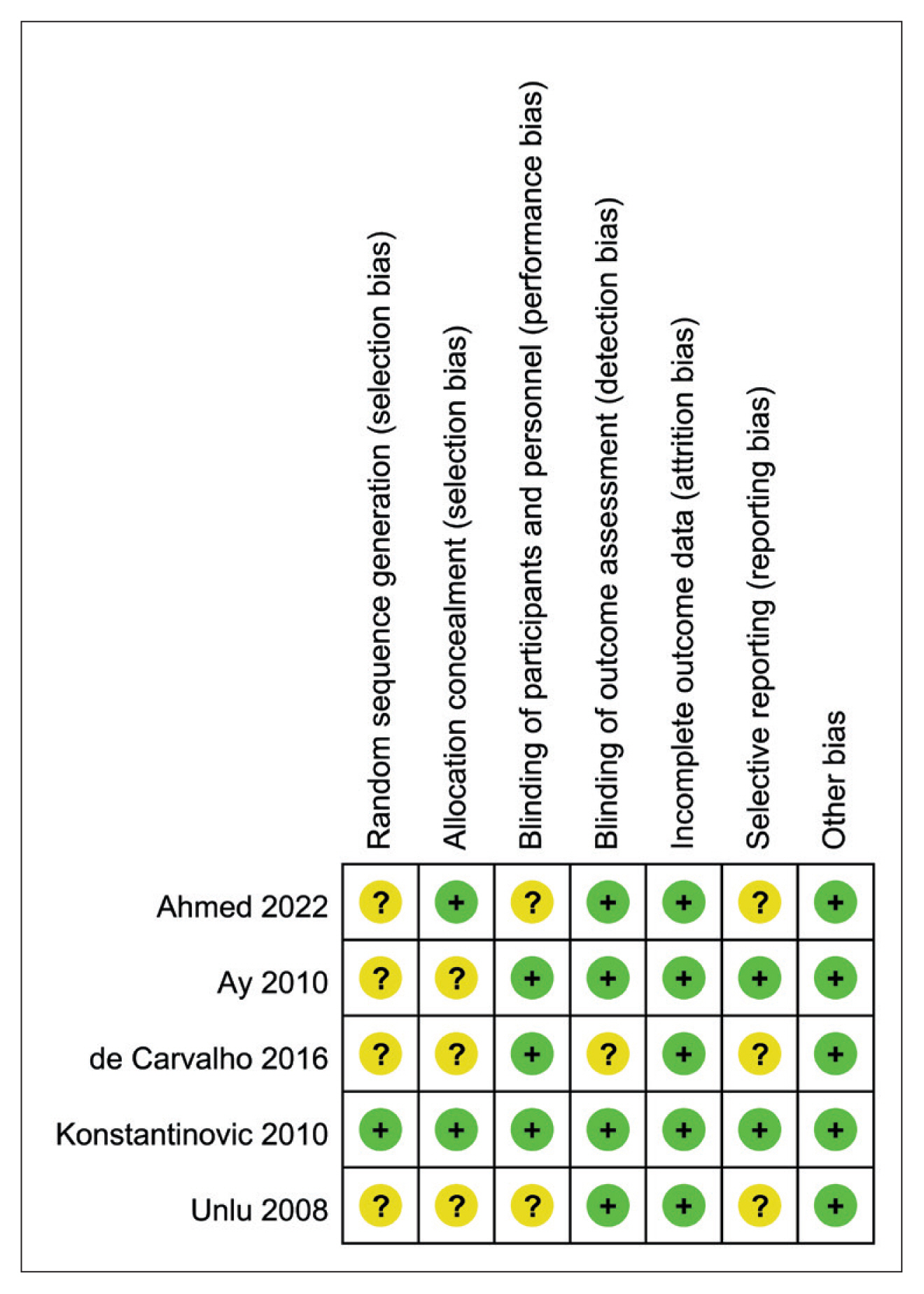
- 3. Risk of bias
- In terms of the random sequence generation domain for the assessment of RoB, only one study [19] described computer-generated random numbers and thus was assessed as “low risk.” The other four studies [18–21] did not have any description of random sequence generation and were assessed as “unclear risk.”
- In terms of the allocation concealment domain, only two studies [19,21] reported on the matter and were assessed as “low risk.” In contrast, the other three studies had no description of the issue and were determined as “unclear risk.”
- In terms of blinding of participants and personnel, three studies using sham LLLT were assessed as “low risk,” and two studies that did not describe the blinding process were assessed as “unclear risk.” In the blinding of the outcome assessment domain, four studies [17,19–21] had descriptions of blinding in the outcome assessment process by separating investigators and assessors; thus, these studies were assessed as “low risk.” One study [18] did not have a specific description of this aspect of blinding and was assessed as an “unclear risk.”
- In terms of incomplete outcome data, studies with no missing values, studies where missing values did not affect the outcomes, and studies where the occurrence of missing values was similar between different intervention groups and the reasons for the occurrence of missing values were similarly assessed as “low risk.”
- In the selective reporting domain, two studies [17,19] that reported AEs were assessed as “low risk,” and the other three did not report AEs and were assessed as “unclear risk.” In the other bias domain, all five selected studies were considered to have no other bias and were assessed as “low risk.”
- A schematic summary of the RoB assessments of the five selected studies is presented in Fig. 2.
- 4. Meta-analysis
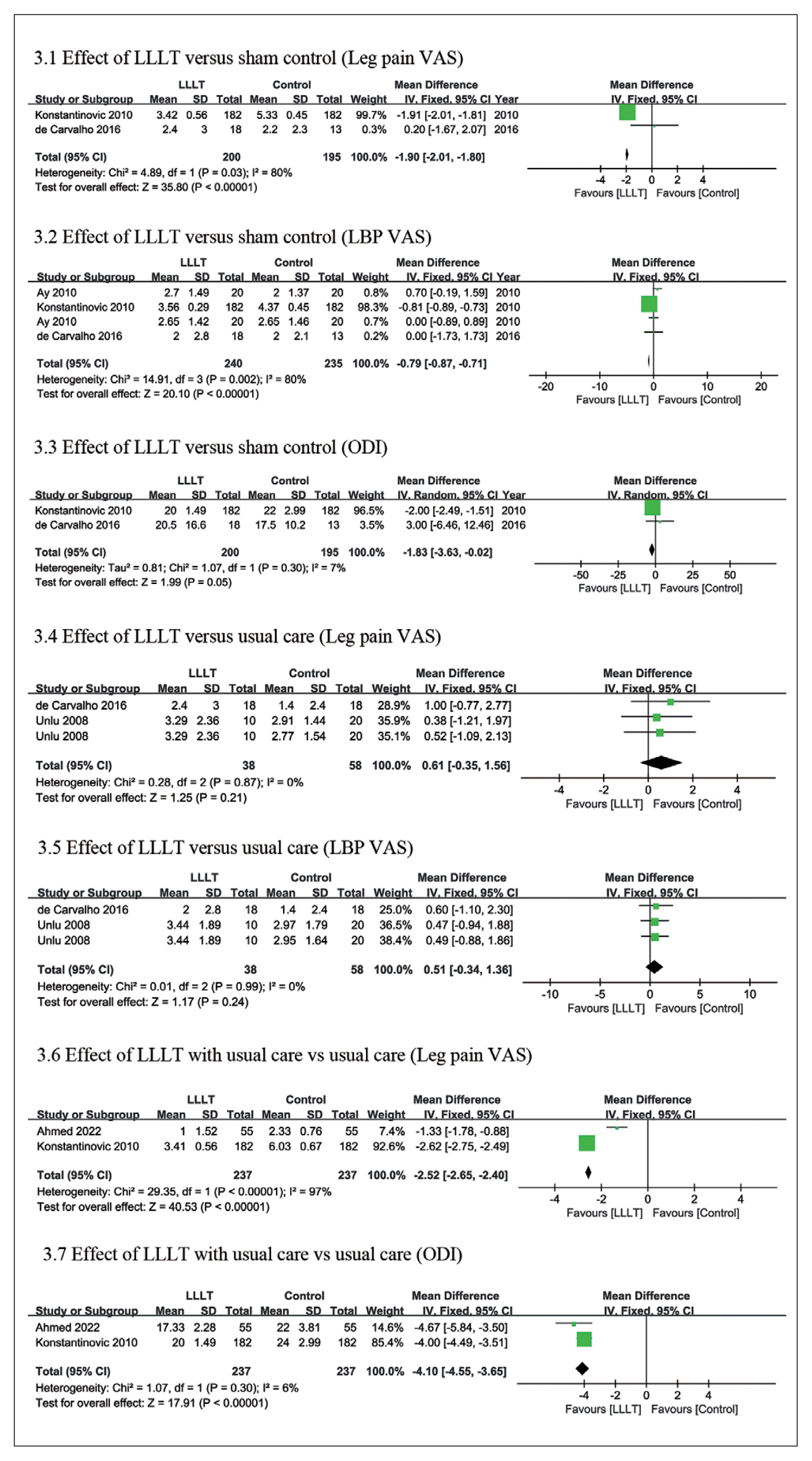
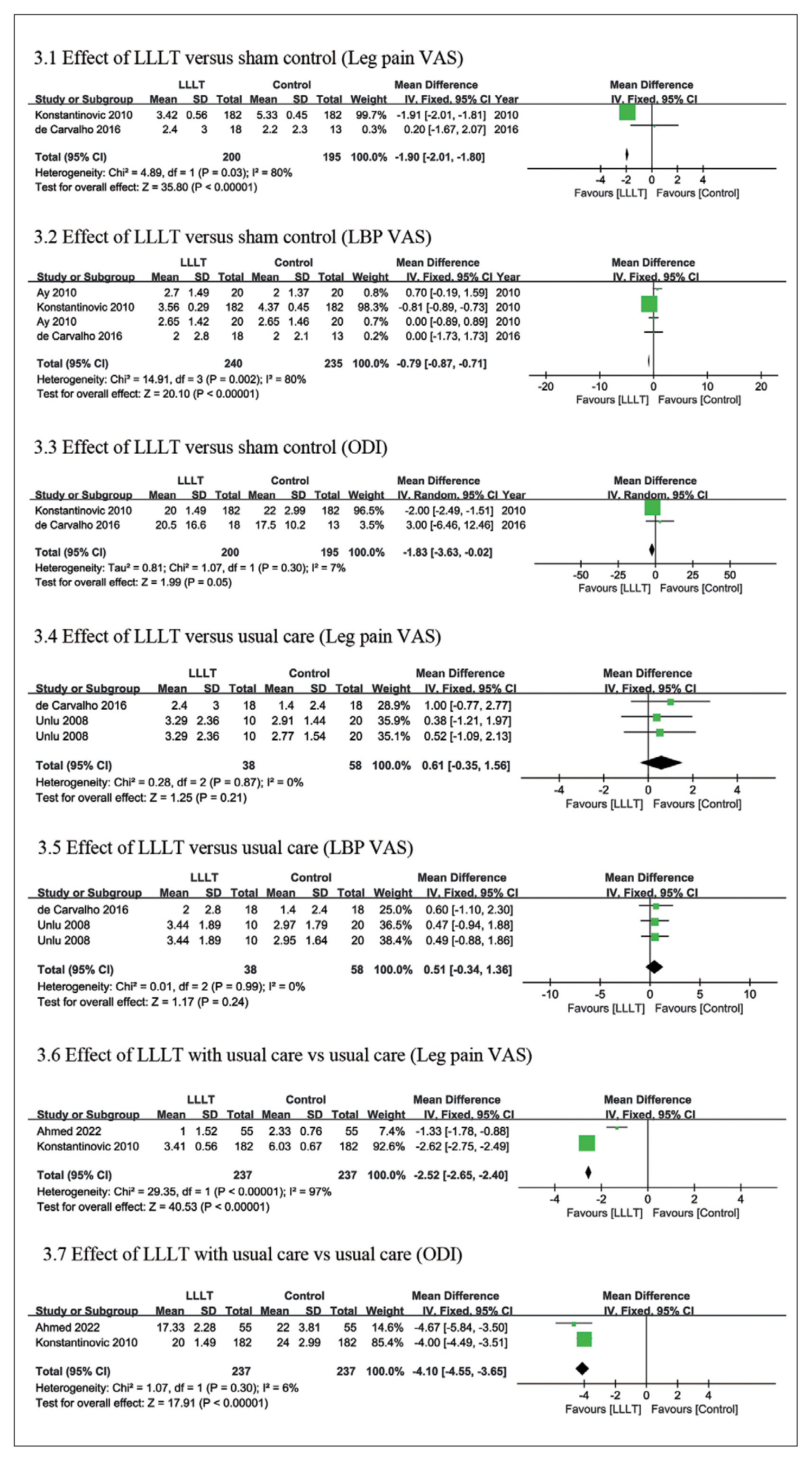
- The meta-analysis on the VAS for leg pain confirmed a significant difference in outcome with an MD of −1.90 [95% confidence interval (CI): −2.01, −1.80]; however, substantial heterogeneity was identified (I2 of 80%). As a result of the meta-analysis on the VAS for LBP, a significant difference in outcome was confirmed with an MD of 0.79 (95% CI: −0.87, −0.71); however, substantial heterogeneity was identified (I2 of 80%). In the meta-analysis on ODI, the MD was −1.83 (95% CI: −3.63, −0.02; Fig. 3).
- As a result of the meta-analysis on the VAS for leg pain, no significant difference in outcome was confirmed with an MD of 0.61 (95% CI: −0.35, 1.56). As a result of the meta-analysis on the VAS for LBP, no significant difference in outcome was confirmed with an MD of 0.51 (95% CI: −0.34, 1.36; Fig. 3). There was no significant difference in the outcomes compared with usual care, such as ultrasound, or physical therapies. ODI was reported in only one study with an MD of −1.90 (95% CI: −13.59, 9.79; data not shown).
- As a result of the meta-analysis on the VAS for leg pain, a significant difference in the outcome of pain reduction was confirmed with an MD of −2.52 (95% CI: −2.65, −2.40). However, considerable heterogeneity was identified (I2 of 97%). As a result of the meta-analysis on the VAS for LBP, the MD was −1.47 (95% CI: −1.58, −1.36); however, only one study reported on this outcome. Meta-analysis of the ODI showed an MD of−4.10 (95% CI: −4.55, −3.65), confirming a significant difference in the outcome of improvement in functional disability (Fig. 3).
- 5. Safety
- Only two studies reported AEs [17,19]. One study described AEs in two patients, which were cases of worsening pain. Of the two patients, one was from the LLLT group, and the other was from the nimesulide and placebo LLLT group [19]. Ay et al [17] reported no AEs.
- 6. Quality of evidence
- The quality of evidence of the articles included in this meta-analysis was assessed according to GRADE methodology-based outcome indicators. In the comparison between LLLT and placebo (sham), leg pain (VAS) was determined to be “very low” owing to RoB, inconsistency, and imprecision, whereas LBP (VAS) and ODI of the quality of evidence were determined to be “low.” In the comparison between LLLT and usual care, the quality of leg pain (VAS), LBP (VAS), and ODI were “low” owing to RoB and imprecision. In the comparison of LLLT with usual care, leg pain (VAS) quality was determined to be “low” owing to RoB and inconsistencies. The quality of evidence for LBP (VAS) and ODI was determined to be “moderate” owing to RoB and imprecision.
Results
2.1. Participants
2.2. Intervention of LLLT
2.3. Controls/comparators
2.4. Outcomes
4.1. LLLT vs. sham control
4.2. LLLT vs. usual care
4.3. LLLT with usual care vs. usual care (add-on)
- Common treatments for LDH include surgery, injection therapy such as epidural steroid injections, and a spectrum of conservative treatments such as medications, and physical therapy [2]. In the case of surgery, as well as the nature of the irreversible treatment, there are risks of complications such as infection and failed back surgery syndrome. Epidural steroid injections are not without risk either, and are associated with a risk of infection or neurologic complications. Therefore, an increasing number of patients choose or prefer conservative treatments with less risk involved [22–24]. Among previous systematic reviews, there have been studies on LLLT for nonspecific chronic LBP [11,25], but few on LLLT for LDH. Therefore, this review was conducted to assess the effectiveness of LLLT for LDH. Effectiveness of LLLT compared with sham treatment of radiculopathy (radiating leg pain) and LBP caused by LDH was observed (although there was substantial heterogeneity); furthermore, its effectiveness in improving functional disability was determined. Owing to the issues of substantial heterogeneity and imprecision of studies, the quality of evidence ranges from “very low” to “low.” However, there was no significant difference in the outcomes compared with usual care, such as ultrasound, or physical therapy such as traction. The analysis revealed a significantly superior improvement in leg pain (although there was substantial heterogeneity) and functional disability when LLLT was applied as an add-on therapy with analgesics or physical therapy, compared with usual care alone. Thus, the findings of this study suggest the possibility of using LLLT as an add-on therapy to conventional conservative treatments.
- No significant direct risks have been reported apart from the following cases: risks related to eyes, including periorbital areas, cases of active cancer cells or suspected carcinoma, and treatment for pregnant women [26]. Of the five studies in this review, two studies [17,19] reported AEs one RCT reported continued pain and one RCT reported no AEs. There were 3 RCTs that did not report on whether any AEs occurred.
- The strength of the study lies in the fact that this is the first systematic review conducted to assess the efficacy and safety of LLLT for LDH in RCTs reported in published literature. However, this study had several limitations. Firstly, the number of studies included in the analysis was small, and most included studies were small-scale RCTs with small sample sizes. The studies in a meta-analysis are homogeneous (in terms of participants, interventions, and outcomes) if they share a common underlying true effect size; otherwise, they are heterogeneous. Secondly, since the laser treatment protocols differed between different RCTs and four of the five studies were aimed at patients with acute LDH, further studies are required to determine whether LLLT is effective in patients with chronic LDH.
- In future studies, additional RCTs designed with more detailed considerations and rigor will be required to accurately assess whether LLLT can be applied as part of the usual care for patients with LDH.
Discussion
- In this systematic review, the effectiveness and safety of LLLT for treating radiologically diagnosed LDH was investigated. LLLT was determined to be more effective than the placebo in alleviating pain and disability in patients with LDH. The outcomes of using LLLT as monotherapy did not significantly differ from that using usual care. In contrast, when LLLT was employed as an add-on therapy with usual care, the studies reported the possibility of significant differences in outcomes. There is limited data regarding safety assessments. As there have been few published studies on the effectiveness and safety of LLLT, we also emphasize the need to establish relevant evidence through well-designed large-scale RCTs in the future.
Conclusion
Supplementary Material
-
Author Contributions
Conceptualization: DN. Data curation: SJL and KBP. Funding acquisition: DN. Investigation: SJL, SJN and JRK. Methodology: SJ. Project administration: YH and DN.
Supervision: KBP, YH and DN. Validation: SJ. Visualization: KBP. Writing - original draft: SJL. Writing - review & editing: YH and DN.
-
Conflicts of Interest
The authors have no conflicts of interest to declare.
-
Funding
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute, funded by the Ministry of Health & Welfare, Republic of Korea (grant no.: HF22C0128).
-
Ethical Statement
No ethical approval was needed for this study.
Article information
Data Availability
| First author (y) | Country | Condition / disease | Intervention group (n) | Comparison group (n) | Main outcomes | Adverse event | Authors conclusion |
|---|---|---|---|---|---|---|---|
| LLLT vs. placebo | |||||||
|
|
|||||||
| Ay (2010) [17] | Turkey | Acute & chronic LDH | LLLT (40) | Sham LLLT (40) |
1) VAS (LBP) 2) Patient’s global assessment 3) Physician’s global assessment 4) Left lateral flexion 5) Modified Schober test 7) RMDQ 8) Modified ODI |
No AEs | No difference |
| De Carvalho (2016) [18] | Brazil | LDH (L4–S1) with radiculopathy | LLLT (18) | Sham LLLT (13) |
1) VAS (LBP) 2) VAS (leg pain) 3) AHFA 4) ODI |
NR | NR |
| Konstantinovic (2010) [19] | Serbia | Acute LBP with radiculopathy by LDH | LLLT (182) | Sham LLLT (182) |
1) VAS (leg pain) 2) VAS (LBP) 3) ODI 4) Schober test 5) PCS 6) MCS |
2 patients (worsening pain) | Laser > sham |
|
|
|||||||
| LLLT vs. usual care | |||||||
|
|
|||||||
| Unlu (2008) [20] | Turkey | Acute LBP with leg pain by LDH | LLLT (20) |
Traction (20) Ultrasound (20) |
1) lateral flexion 2) Shober test 3) Muscular tenderness 4) Positive SLR 5) VAS (LBP) 6) VAS (leg pain) 7) RMDQ 8) Modified ODI 9) Size of the herniated mass on MRI |
NR | Generally, no difference |
| De Carvalho (2016) [18] | Brazil | LDH (L4–S1) with radiculopathy | LLLT (18) | LED (18) |
1) VAS (LBP) 2) VAS (leg pain) 3) AHFA 4) ODI |
NR | LED > LT |
|
|
|||||||
| LLLT with usual care versus usual care (add-on) | |||||||
|
|
|||||||
| Konstantinovic (2010) [19] | Serbia | Acute LBP with radiculopathy by LDH | LLLT + nimesulide (182) | Nimesulide (182) |
1) VAS (leg pain) 2) VAS (LBP) 3) ODI 4) Schober test 5) PCS 6) MCS |
2 patients (worsening pain) | LLLT + nimesulide > nimesulide |
| Ahmed (2022) [21] | Pakistan | Acute LBP with unilateral radiculopathy by LDH | LLLT + physical therapy (55) | Physical therapy (55) |
1) VAS (leg pain) 2) ODI 3) Lumbar flexion 4) Lumbar extension |
NR | LLLT + physical therapy > physical therapy |
LBP = lower back pain; LDH = Lumbar disc herniation; LLLT = low-level laser treatment; VAS = visual analog scale; RMDQ = Ronald Morris disability questionnaire; AHFA = affected hip flexion angle; ODI = Oswestry Disability Index; PCS = physical component summary; MCS = mental component summary; NR. = not reported; AE = adverse event; MRI = magnetic resonance imaging.
| First author (y) | Medium (model, manufacturer) | Wavelength (nm) / type | Power output (mW) / power density (mW/cm2) | Energy density (J/cm2) / dose/point (J/point) | Beam size / No. of treatments / treatment time | Treatment sessions & interval |
|---|---|---|---|---|---|---|
| Ay (2010) [17] | GaAlAs (Chattanooga group, USA) | 850 / continuous | 100 / NR | 40 / NR | 0.07 cm2/ 2–4 points (both sides of the paraspinal tissues of the disk spaces) / 4 m/point | 15 ×, 5 × / wk, 3 wks |
| De Carvalho (2016) [18] | AsGa (HTM brand, São Carlos, SP, Brazil) | 904 / pulse type (pulse rate 5 KHz) | 38 / 238 | 0.23 / 4 | 0.16 cm2 / 20 points (12 points: L2–S1 + 8 points: thigh in the path of L5 and S1) / 104 s/point | 15 ×s, 5 × / wk, 3 wks |
| Konstantinovic (2010) [19] | NR (Enraf Nonius, Rotterdam, The Netherlands) | 904 / pulse type (pulse rate 5,000 Hz) | 100 / 20 | 3 / 3 | 1 cm2 / 4 points (local transforaminal) / 150 s/point | 15 ×, 5 × a wk |
| Unlu (2008) [20] | Gal-Al-As (Endolaser 476, Enraf Nonius)) | 830 / continuous | 50 / NR | NR / 1 | 1 mm (diameter) / both sides of the disc spaces where herniation was detected on MRI / 4 m/point | 15 ×, 5 × / wk, 3 wks |
| Ahmed (2022) [21] | NR | 830 / NR | 100/ 0.67 W/cm2 or 300 mW/cm2 | 3/3 | 1 cm/ 4 points/30 s/point | 18 ×, 3 × / wk for 6 or 8 wks |
- [1] Hurwitz EL, Randhawa K, Yu H, Côté P, Haldeman S. The Global Spine Care Initiative: a summary of the global burden of low back and neck pain studies. Eur Spine J 2018;27(Suppl 6):796−801.ArticlePubMedPDF
- [2] Kreiner DS, Hwang SW, Easa JE, Resnick DK, Baisden JL, Bess S, et al. An evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy. Spine J 2014;14(1):180−91.ArticlePubMed
- [3] Jeong HSSY, Lee KS. Aging and Health Care Expenditure. Korean J Health Econ Policy 2007;13:95−116. https://www.kci.go.kr/kciportal/ci/sereArticleSearch/ciSereArtiView.kci?sereArticleSearchBean.artiId=ART001058606.
- [4] Park YHJ, Park HY, Shim M, Shin BR. [Internet]. A study on spinal disease compartment according to lifestyle and behavior using National Health Insurance data: 2015 Available from: http://lib.nhis.or.kr/search/detail/CAT000000024644
- [5] AlGhamdi KM, Kumar A, Moussa NA. Low-level laser therapy: a useful technique for enhancing the proliferation of various cultured cells. Lasers Med Sci 2012;27(1):237−49.ArticlePubMedPDF
- [6] Peplow PV, Chung TY, Baxter GD. Laser photobiomodulation of wound healing: a review of experimental studies in mouse and rat animal models. Photomed Laser Surg 2010;28(3):291−325.ArticlePubMed
- [7] Chung H, Dai T, Sharma SK, Huang YY, Carroll JD, Hamblin MR. The nuts and bolts of low-level laser (light) therapy. Ann Biomed Eng 2012;40(2):516−33.ArticlePubMedPMCPDF
- [8] Chow RT, Johnson MI, Lopes-Martins RA, Bjordal JM. Efficacy of low-level laser therapy in the management of neck pain: a systematic review and meta-analysis of randomised placebo or active-treatment controlled trials. Lancet 2009;374(9705):1897−908.ArticlePubMed
- [9] Bjordal JM, Johnson MI, Iversen V, Aimbire F, Lopes-Martins RA. Low-level laser therapy in acute pain: a systematic review of possible mechanisms of action and clinical effects in randomized placebo-controlled trials. Photomed Laser Surg 2006;24(2):158−68.ArticlePubMed
- [10] Bjordal JM, Couppé C, Chow RT, Tunér J, Ljunggren EA. A systematic review of low level laser therapy with location-specific doses for pain from chronic joint disorders. Aust J Physiother 2003;49(2):107−16.ArticlePubMed
- [11] Hakgüder A, Birtane M, Gürcan S, Kokino S, Turan FN. Efficacy of low level laser therapy in myofascial pain syndrome: an algometric and thermographic evaluation. Lasers Surg Med 2003;33(5):339−43.ArticlePubMed
- [12] Huang Z, Ma J, Chen J, Shen B, Pei F, Kraus VB. The effectiveness of low-level laser therapy for nonspecific chronic low back pain: a systematic review and meta-analysis. Arthritis Res Ther 2015;17:360. ArticlePubMedPMC
- [13] Glazov G, Yelland M, Emery J. Low-level laser therapy for chronic non-specific low back pain: a meta-analysis of randomised controlled trials. Acupunct Med 2016;34(5):328−41.ArticlePubMedPMCPDF
- [14] Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009;339:b2700. ArticlePubMedPMC
- [15] Kim SY, Park JE, Seo HJ, Lee YJ, Jang BH, Son HJ, et al. [Intenret]. NECA’s guidance for undertaking systematic reviews and meta-analyses for intervention: Nataional Evidence-based Healthcare Collaborating Agency: 2011 Available from: http://lib.nhis.or.kr/search/detail/CAT000000006943
- [16] Balshem H, Helfand M, Schünemann HJ, Oxman AD, Kunz R, Brozek J, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 2011;64(4):401−6.ArticlePubMed
- [17] Ay S, Doğan SK, Evcik D. Is low-level laser therapy effective in acute or chronic low back pain? Clin Rheumatol 2010;29(8):905−10.ArticlePubMedPDF
- [18] de Carvalho ME, de Carvalho RM Jr., Marques AP, de Carvalho Lucio LM, de Oliveira AC, Neto OP, et al. Low intensity laser and LED therapies associated with lateral decubitus position and flexion exercises of the lower limbs in patients with lumbar disk herniation: clinical randomized trial. Lasers Med Sci 2016;31(7):1455−63.ArticlePubMedPDF
- [19] Konstantinovic LM, Kanjuh ZM, Milovanovic AN, Cutovic MR, Djurovic AG, Savic VG, et al. Acute low back pain with radiculopathy: a double-blind, randomized, placebo-controlled study. Photomed Laser Surg 2010;28(4):553−60.ArticlePubMed
- [20] Unlu Z, Tasci S, Tarhan S, Pabuscu Y, Islak S. Comparison of 3 physical therapy modalities for acute pain in lumbar disc herniation measured by clinical evaluation and magnetic resonance imaging. J Manipulative Physiol Ther 2008;31(3):191−8.ArticlePubMed
- [21] Ahmed I, Bandpei MAM, Gilani SA, Ahmad A, Zaidi F. Effectiveness of Low-Level Laser Therapy in Patients with Discogenic Lumbar Radiculopathy: A Double-Blind Randomized Controlled Trial. J Healthc Eng 2022;2022:6437523. ArticlePubMedPMCPDF
- [22] Hiratzka J, Rastegar F, Contag AG, Norvell DC, Anderson PA, Hart RA. Adverse Event Recording and Reporting in Clinical Trials Comparing Lumbar Disk Replacement with Lumbar Fusion: A Systematic Review. Global Spine J 2015;5(6):486−95.ArticlePubMedPMCPDF
- [23] Eworuke E, Crisafi L, Liao J, Akhtar S, Van Clief M, Racoosin JA, et al. Risk of serious spinal adverse events associated with epidural corticosteroid injections in the Medicare population. Reg Anesth Pain Med 2021;46(3):203−9.ArticlePubMed
- [24] Epstein NE. Neurological complications of lumbar and cervical dural punctures with a focus on epidural injections. Surg Neurol Int 2017;8:60. ArticlePubMedPMC
- [25] Yousefi-Nooraie R, Schonstein E, Heidari K, Rashidian A, Pennick V, Akbari-Kamrani M, et al. Low level laser therapy for nonspecific low-back pain. Cochrane Database Syst Rev 2008;2008(2):CD005107. ArticlePubMedPMC
- [26] Filshie J, White A, Cummings M. Medical Acupuncture: A Western Scientific Approach. Elsevier, 2016.




 PubReader
PubReader ePub Link
ePub Link Cite
Cite