Articles
- Page Path
- HOME > Perspect Integr Med > Volume 2(2); 2023 > Article
-
Review Article
Minimum Clinically Important Difference for Nonsurgical Interventions for Spinal Diseases: Choosing the Appropriate Values for an Integrative Medical Approach -
Ye-Seul Lee
 , Sungmin Lee
, Sungmin Lee , Yoon Jae Lee
, Yoon Jae Lee , In-Hyuk Ha*
, In-Hyuk Ha*
-
Perspectives on Integrative Medicine 2023;2(2):86-99.
DOI: https://doi.org/10.56986/pim.2023.06.003
Published online: June 23, 2023
Jaseng Spine and Joint Research Institute, Jaseng Medical Foundation, Seoul, Republic of Korea
- *Corresponding author: In-Hyuk Ha, Jaseng Spine and Joint Research Institute, Jaseng Medical Foundation, Seoul 06110, Republic of Korea, Email: hanihata@gmail.com
©2023 Jaseng Medical Foundation
This is an open access article under the CC BY-NC license (http://creativecommons.org/licenses/by-nc/4.0/).
- 910 Views
- 26 Download
- 2 Crossref
Abstract
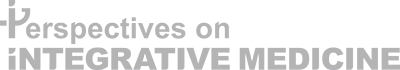
- The minimal clinically important difference (MCID) plays a crucial role in the design and interpretation of clinical trials, as it helps in distinguishing between statistically significant and clinically meaningful outcomes. This scoping review aims to collate and appraise the current research concerning the validation of MCIDs for surgical and nonsurgical measures for spine disorders. Two databases of MEDLINE (PubMed and EMBASE) were searched. There were 1,590 studies retrieved and 79 were selected as eligible for review. Measurement tools such as the Oswestry Disability Index, Neck Disability Index, Numeric Rating Scale, and Visual Analogue Scale were assessed by regions and interventions. A total of 24 studies identified MCIDs on nonsurgical interventions, and 55 studies identified MCIDs on surgical interventions. The range of MCIDs varied greatly depending on study population, specific interventions, calculation methods, and outcomes. This scoping review emphasizes the complexity and variability in determining MCIDs for musculoskeletal or neurodegenerative spinal diseases, influenced by several factors including the intervention type, measurement tool, patient characteristics, and disease severity. Given the wide range of reported MCIDs, it is crucial to consider the specific context when interpreting these values in clinical and research settings. To select an appropriate MCID value for comparison in a clinical trial, careful consideration of the patient group, intervention, assessment tools, and primary outcomes is necessary to ensure that the chosen MCID aligns with the research question at hand.
- Minimal clinically important difference (MCID) is an extensively used tool in healthcare clinical trials, and is defined as “the smallest difference in score in the domain of interest which patients perceive as beneficial [1].” Reporting the results using MCIDs is easily interpretable and efficient, particularly in clinical trials employing patient reported outcomes. Due to its usefulness, a vast range of studies have utilized this concept since its introduction [2]. By providing a statistical measure to assess the effectiveness of clinical interventions, this concept is particularly relevant in the field of spine disorders, where both surgical and nonsurgical treatments are employed to alleviate pain and improve patient function, and where patient reported outcomes comprise a substantial portion of the outcomes. The evaluation and validation of MCIDs in these interventions are vital to ensure appropriate patient care, as well as to determine the effectiveness of new and existing treatments.
- Surgical and nonsurgical treatments for spine disorders encompass a wide range of interventions. Surgical measures often include procedures such as spinal fusion, discectomy, laminectomy, and foraminotomy, among others. On the other hand, nonsurgical interventions may involve physical therapy, pain management (including medication and injections), lifestyle modifications, and complementary and alternative medicine approaches including acupuncture and Tuina (Chuna). The MCID values for these interventions can differ significantly, and the wide range of recommended MCID values for the same instrument [3,4] highlights the need for context-specific validation.
- Determining the MCID is not a straightforward process, and various methods are employed to derive these values. Anchor-based approaches, distribution-based techniques, and receiver operating characteristic (ROC) curve analysis represent the most common methods used for MCID validation. Anchor-based approaches use an external criterion or “anchor” to interpret the meaning of a change in the outcome measure, whereas distribution-based methods relate the observed changes to the variability of the measure. ROC curve analysis provides an alternative method, utilizing sensitivity and specificity to assess the cut-off point that best differentiates between improvement and no improvement in patient symptoms.
- Each of these methods carries inherent strengths and weaknesses, and their use often depends on the context and the nature of the intervention under study. However, there is currently no consensus on which method is the most appropriate or accurate for validating MCIDs in the context of spine disorders. Discrepancies between anchor-based and distribution-based MCIDs [5] have been reported, and the lack of agreement poses challenges for clinicians and researchers in the interpretion of clinical trial results and in making informed decisions about patient care.
- The MCID plays a crucial role in the design and interpretation of clinical trials, as it helps in distinguishing between statistically significant and clinically meaningful outcomes. Without a proper MCID, the results of clinical trials can be misleading, and interventions that are statistically effective may not translate into meaningful improvements in patient outcomes. Differences in the range of MCIDs for the same disease have been observed by interventions [6], implying the need to review the related literature. An appropriately selected MCID can provide guidance in clinical decision-making by helping to quantify the benefits and harms of different interventions.
- This scoping review aimed to address the existing knowledge gap by collating and critically appraising the current body of research concerning the validation of MCIDs for surgical and nonsurgical measures for spine disorders. It will provide a comprehensive overview of the current methods of MCID validation, highlight the most common surgical and nonsurgical measures, and underscore the importance of determining the most appropriate MCID in the context of clinical trials. In doing so, this review hopes to contribute to the ongoing discourse and pave the way for more robust and patient-centered approaches in the management of spine disorders.
Introduction
- This scoping review was designed to identify MCIDs for musculoskeletal disorders and neurodegenerative diseases of the spine. A scoping review is a form of knowledge synthesis that addresses exploratory research questions that try to map significant concepts, types of evidence, and research gaps pertaining to a given topic or field by finding, collecting, and synthesizing existing knowledge [7]. This study followed the method based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) extension for scoping reviews [8] The following five steps were used to conduct this scoping review: (1) identification of the research question; (2) identification of relevant studies; (3) study selection; (4) charting of data; and (5) collecting, summarizing, and reporting the results as described by Peters et al [9]. This study followed the method based on the Arksey and O’Malley framework [10].
- 1. Identifying the research questions
- Prior to the initiation of this study, the broad research question was “what are the differences between MCIDs for nonsurgical interventions and those for surgical interventions in spinal diseases?” The more detailed research questions used after starting the study were as follows: (1) What is the difference in the reported MCID across various types of interventions (i.e., surgical and nonsurgical interventions) for spine disorders? (2) How do different methods of study design impact the reported MCID values for spine disorders? (3) Are there any cultural or geographical factors that may influence MCIDs? (4) What is the difference in the choice of patient-reported outcome measures across reported MCIDs in surgical and nonsurgical interventions for spine disorders? and (5) Considering the MCID values reported, how might the choice of treatment intervention and outcome measurement instruments influence the interpretation of clinical significance in studies of surgical and nonsurgical interventions for spine disorders?
- 2. Identifying the relevant studies
- The initial search was conducted using the two electronic databases of MEDLINE, via PubMed and Excerpta Medical dataBASE (EMBASE). An example of the specific search strategy is listed in Table 1. Modifications to the search terms and search strategies were adopted in reference to the database being searched.
- 3. Study selection
- This study reviewed studies which assessed MCIDs for spinal diseases treated by surgical or nonsurgical interventions. Human studies including randomized controlled trials, controlled clinical trials, case series, case reports, pilot clinical studies, and retrospective observational studies were reviewed for eligibility. In vivo and in vitro experiments, reviews, duplicate articles, ongoing studies, and studies that failed to provide detailed results or with incomplete data were excluded. The language was restricted to English, and time period was restricted to studies published since 1989 when the concept of MCID was first introduced [1]. An elaborate search criteria is listed in Supplementary Table 1.
- Eligible participants were defined as patients with spinal disease who were: (1) over 18 years of age; (2) who were, or had been, going through treatment for musculoskeletal or neurodegenerative disorders in the neck or back; and (3) who received either surgical or nonsurgical interventions to address the symptoms. Patients experiencing other types of disorders such as tumor or autoimmune diseases such as ankylosing spondylitis were excluded from this scoping review. No restriction was applied according to sex, ethnicity, symptom severity, disease duration, clinical setting, and country of study.
- Examples of surgical interventions in this study include discectomy, disc replacement, laminectomy, fusion, and/or decompression surgery. Examples of nonsurgical interventions in this study include physical therapy, exercise and education programs, spinal cord stimulation, and complementary and alternative medicine therapies such as acupuncture and Tuina (Chuna).
- The outcomes collected and reviewed in this study were MCIDs across a number of assessment measurements, including the Oswestry Disability Index (ODI), Patient-Reported Outcomes Measurement Information System Physical Function (PROMIS-PF), EuroQol 5-dimensions (EQ-5D), Numeric Rating Scale (NRS) for different types of pain, and Visual Analogue Scale (VAS) for pain.
- The electronic databases were searched independently by two researchers using the search strategies described above and the retrieved studies were screened for eligibility. Upon the initial search, all citations were uploaded to EndNote X20 (Clarivate Analytics, Philadelphia, PA, USA). After removing the duplicates, full texts were reviewed in detail using the inclusion criteria. The number of results for each database search was noted and presented in a PRISMA flow diagram. The reasons for excluding studies were recorded for individual studies.
- As this review focused on comparing the reported MCIDs and the methods used to validate the MCID, the study information assessed for this review were as follows: the 1st author, corresponding author, publication year, country, language, study type, patient disease, type of intervention(s), outcome measures, primary outcome, secondary outcome, reported MCIDs, and statistical analysis method. Data extraction was performed independently by two researchers and any differences were resolved through discussion. The data charting table was modified as necessary during the process of data extraction.
- After coding the included studies, the contents of the studies were analyzed. The extracted data were presented in tabular form in line with the objective of this scoping review. The distribution of the studies by the aforementioned extracted information was analyzed. A qualitative analysis was conducted to illustrate an overview of each study. The tabulated results were supported by narrative summaries to describe the results in relation to the objective of this scoping review.
Materials and Methods
3.1. Inclusion/exclusion criteria
3.2. Screening and agreement
3.3. Charting the data
3.4. Collecting, summarizing, and reporting the results
- 1. Literature search and selection
- Based on the search strategy, a total of 1,590 studies published on MCIDs for spinal diseases were retrieved from PubMed and EMBASE. After title and abstract screening, a total of 604 studies were assessed for eligibility. After the assessment of full-text, a total of 489 studies were excluded for the following reasons: RCTs on the effectiveness of specific interventions (n = 331), studies on autoimmune diseases and/or metastatic diseases (n = 29), studies on risk factors for spine disease prognosis (n = 139), and instrument validation (n = 24). A total of 79 studies were included for this scoping review. The PRISMA flow chart was used to track the number of articles at each stage of the review (Fig. 1).
- 2. General characteristics of the identified literature
- A total of 79 studies were reviewed in this study (Supplementary Table 2). They were conducted between 2004 and 2022, and the number of studies showed an increasing trend over the years (Fig. 2). The largest number of studies (10 articles) were published in 2019. Research was conducted in various regions including the USA, Japan, Switzerland, Norway, Sweden, Thailand, Belgium, Turkey, Canada, Iran, the Republic of Korea, Denmark, Spain, and China. Multiple study designs were present, but most of them were based on observational study designs including retrospective or prospective cohort studies. Other study designs included a case-control study and secondary analysis of a randomized controlled trial.
- MCIDs for nonsurgical interventions using various assessment tools or instruments were identified in 24 studies (Table 2). The interventions assessed in these studies were diverse, encompassing physical therapy, pain medication, exercise and education programs, spinal cord stimulation, acupuncture, Chuna (Tuina), cupping, and other rehabilitation programs. A wide array of instruments have been used across these studies to measure treatment outcomes, and commonly used tools include PROMIS-29, neck disability index (NDI), SF-12, NPS, and ODI.
- MCIDs for surgical interventions using various assessment tools or instruments were identified in 55 studies (Supplementary Table 3). Spinal conditions included spinal conditions in the neck and back, including degenerative cervical myelopathy, cervical radiculopathy, lumbar spinal stenosis, and lumbar degenerative disc disease, among others. Interventions encompassed discectomy, disc replacement, laminectomy, and fusion and decompression surgery.
- Instruments used to measure outcomes included ODI, PROMIS-PF, Japanese Orthopaedic Association score, NRS and VAS for various types of pain, health-related quality of life assessment measurements such as Short Form (SF)-36 survey, and EQ-5D, and tests such as the timed-up-and-go (TUG) test, and 6-minute walk distance. MCIDs for some instruments, e.g., PROMIS, the Beck Depression Inventory, and the Tampa Scale of Kinesiophobia was determined only for nonsurgical treatments. On the other hand, MCIDs for certain instruments such JOABPEQ was determined only for surgical treatments.
- Anchor-based, distribution-based, ROC analysis, or a combination approach were used to determine the MCIDs. The reported MCID values varied significantly across the studies, interventions, and instruments used. For example, the MCID for the TUG test conducted by Maldaner et al in 2022 [11] on patients who had gone through lumbar disc surgery was 2.1 seconds. In contrast, the MCID for the TUG test conducted by Gautschi et al [12] in 2017 on patients who had gone through microdiscectomy was 3.4 seconds. Similarly, the MCID for the ODI ranged from 9 [13] to above 26.6 [14].
- 3. Reported MCIDs by instruments and by interventions
- When MCIDs of the ODI were assessed by interventions (Table 3), MCIDs across nonsurgical interventions, reported in eight studies [5,13,15–18], ranged between 2.23–14.31 [15] on pain medication. Studies which calculated a single value ranged from 2.45 [19] on a composite of nonsurgical procedures for adult spine deformity and 9 [13] on acupuncture and Chuna (Tuina) for failed back surgery syndrome (FBSS), or a minimum of 50% change for physical therapy using the ODI [20]. MCIDs across surgical interventions for the back, reported in 20 studies [14,15,19,21–37], ranged from 0.17 [30] on fusion surgery to 27 [37] on discectomy, or a minimum of 42.4% change for decompression surgery [22].
- MCIDs for the NDI were assessed by interventions (Table 4). MCIDs across nonsurgical interventions, reported in ten studies [5,38–45], and ranged from 1.66 [45] for physiotherapy with manual therapy techniques to 18 [5] on a composite of nonsurgical treatment for spine disorders. The change in the NDI for physical training ranged from 20% to 60%. MCIDs across surgical interventions on the neck, reported 20–60% in 8 studies [46–53], ranged from 2.72–12.08 [51]. When assessing symptom change, one study on physical training reported 20–60% change in the NDI [40] while studies on discectomy and fusion surgery reported a 16% [46] to 30% [47] improvement for degenerative cervical diseases.
- MCIDs for the NRS and VAS were assessed by interventions and by regions (Supplementary Table 4). Five studies [38,39,42–44] reporting NRS/VAS scores for neck pain from nonsurgical treatments ranged from 1.3 [43] to 2.5 [38,44] in NRS. One study on nonsurgical interventions for the neck reported NRS scores for arm pain with an MCID of 1.5 [54]. Five studies reporting NRS/VAS scores for back pain from nonsurgical treatments ranged from improvements in scores of between 1.2 to 3.7 in the VAS [17], and from 0.9 [16] to 4 [18] in the NRS. Seven [46,47,49,52,53,55,56] studies reporting NRS/VAS scores for neck pain from surgical treatments ranged from as low as 0.36 [56] to 2.6 [52] in the VAS. Symptom change ranged from 16% [46] to 30%[47]. Five [47,49,52,53,55] studies reporting NRS/VAS scores for arm pain from surgical treatments ranged from 1.3 [49] to 4.1 [52], and a minimum of 30% change in symptom [47]. Nineteen studies reporting NRS/VAS scores for back pain ranged from 0.02 [30] to 4.2 [14] in the NRS, and 1.16 [31] to 6.5 [33] in the VAS. The NRS score change for back pain ranged from 25% [22] to 33% [27]. Fourteen studies [14,22,23,27–33,35,36,57,58] reported MCIDs for leg pain from surgical treatments for the back, ranging from 0.02 [30] to 3.5 [29,57] in NRS scores, with changes ranging from 40% [27] to 55.60% [22]. Lastly, two studies reported MCIDs for NRS scores for leg numbness, ranging from 2 [57] to 3.75 [22].
Results
- This comprehensive scoping review of 79 studies, spanning 18 years of research, provides an in-depth evaluation of the available literature on the MCID for both non-surgical and surgical interventions in spinal diseases. The studies were conducted across a broad geographical range, indicating a global interest in this topic. The findings highlight the complexity of determining the MCID, with a broad range of values reported across different studies, interventions, calculation methods, measurement tools, and patient populations.
- Notably, the use of numerous assessment tools across studies suggests that there is no consensus on a standardized tool for measuring treatment outcomes in spinal diseases. This variety of instruments used across studies may contribute to the significant variation in the MCID values reported. PROMIS-29 [5,49,59–61], NDI [5,11–14,16,19,20,22–32,35,36,38–54,56,58,61–78], SF-12 and SF-36 [13,19,22,30–36,42,49–53,56,57,60,62,69,72,78–80], NRS [14,16,18,22,25,27,29,43,44,46,47,54,57,64], and ODI [5,12–27,29–37,42,47,48,52,59,60,66,70,71,74,81,82] were common assessment tools, but their application varied, indicating that the choice of instrument may be context-specific. Some tools like PROMIS [5,49,59–61], the Beck?Depression Inventory [16,17], and the Tampa Scale of Kinesiophobia [83] were only used for non-surgical treatments, while others [58,70] were specific to surgical treatments. This suggests further research is needed to establish the suitability of specific tools for different interventions and conditions.
- The methods used to calculate the MCID, including anchor-based, distribution-based, and ROC analysis, or a combination thereof, varied across studies. The diverse methodologies employed may also contribute to the variability in reported MCID values. The difference in MCID values for the same measurement tool, for example, the TUG test [11,12,41], emphasizes the influence of the study population and the specific intervention on the MCID.
- A wide range of MCIDs were observed in this study, even within the same intervention. For example, the MCID for the ODI across non-surgical interventions ranged from 2.23 to 14.31 in relation to pain medication, and from 0.17 to 27 for surgical interventions like fusion surgery, and discectomy. This variability reflects the influence of specific patient characteristics, disease severity, and intervention specifics, further indicating that the MCID is highly context-dependent.
- The same variability was seen in MCIDs for the NDI across interventions, where values ranged from 1.66 on physiotherapy with manual therapy techniques, to 18 on a composite of non-surgical treatment for spine disorders. Regarding pain assessments, a wide range of MCID values for the NRS and VAS were reported. The values ranged from as low as 0.02 to as high as 4.2 for back pain following surgical interventions. This suggests a potential influence of the type and combination of treatments on the MCID, further underscoring the variability in MCIDs depending on the specific intervention and patient population.
- In conclusion, this scoping review highlights the growing body of research on MCIDs over time across various spinal diseases. The result emphasizes the complexity and variability in determining MCIDs for spinal diseases, which are influenced by several factors including the type of intervention, measurement tools, patient characteristics, and disease severity. Given the wide range of reported MCIDs, it is crucial to consider the specific context when interpreting these values in clinical and research settings. This study points to the importance of selecting the most appropriate value of MCID in clinical research as well as in clinical practice of spinal diseases. To select an appropriate MCID value for comparison in a clinical trial, careful consideration of the patient group, intervention, assessment tools, and primary outcomes is necessary to ensure that the chosen MCID aligns with the research question at hand. The findings also underscore the need for further research to understand the influences driving these variations when determining MCIDs. Further effort would be beneficial for both clinical decision-making, and for the design and interpretation of research studies in this field.
Discussion
Supplementary Material
-
Author Contributions
Conceptualization: YSL. Formal analysis: SL and YSL. Methodology: YJL. Project administration: IHH. Writing original draft: YSL. Writing-reveiw and editing: YJL.
-
Conflicts of Interest
The authors have no conflicts of interest to declare.
-
Ethical Statement
This research is literature review that does not require IRB approval.
-
Funding
This research article did not receive any financial funding.
-
Data Availability
All relevant data are included in this manuscript.
Article information

| Authors [ref] | Country | Year | Design | Method | Region | Disease | Intervention | Instruments | Reported MCID |
|---|---|---|---|---|---|---|---|---|---|
| Physiotherapy | |||||||||
|
|
|||||||||
| Khutok et al [61] | Thailand | 2021 | Prospective cohort | Anchor-based | Back | Low back pain | Physical therapy | PROMIS-29 | 0.5 |
|
|
|||||||||
| Young et al [38] | USA | 2019 | Secondary analysis of an RCT | ROC & anchor-based | Neck | Neck pain with cervicogenic headaches | Thoracic manipulation mobilization & exercise | NRS | 2.5 |
| NDI | 3.5 – 5.5 | ||||||||
|
|
|||||||||
| Young et al [39] | USA | 2019 | Secondary analysis of an RCT | ROC & anchor-based | Neck | Neck pain without concomitant upper extremity symptoms | High velocity low-amplitude thrust manipulation or non-thrust mobilization to the upper cervical (C1-2) & upper thoracic (T1-2) spine | NRS | 1.5 |
| NDI | 5.5 | ||||||||
|
|
|||||||||
| Jørgensen et al [40] | Denmark | 2017 | Secondary analysis of an RCT | Anchor-based | Neck | Chronic neck pain | Physical training | NDI | 20–60% |
|
|
|||||||||
| Díaz-Arribas et al [80] | Spain | 2017 | Prospective cohort | Anchor-based | Back | Low back pain | Physical therapy | SF-12 MCS | 3.77 |
| SF-12 PCS | 3.29 | ||||||||
|
|
|||||||||
| Pereira et al [41] | Portugal | 2015 | Prospective cohort | Anchor-based | Neck | Chronic neck pain | Physical therapy | NDI | 5.5 |
|
|
|||||||||
| Young et al [75] | USA | 2009 | Prospective cohort | Anchor-based | Neck | Mechanical neck disorders | Physical therapy | NDI | 7.5 |
|
|
|||||||||
| Fritz et al [20] | USA | 2009 | Prospective cohort | Anchor-based | Back | Low back pain | Physical therapy | ODI | 50% |
|
|
|||||||||
| Cleland et al [43] | USA | 2008 | Prospective cohort | ROC & anchor-based | Neck | Neck pain | Underwent 1 PT treatment session consisting of manual therapy | NRS | 1.3 |
| NDI | 19% | ||||||||
|
|
|||||||||
| Kovacs et al [54] | Spain | 2008 | Retrospective chart review | ROC & anchor-based | Neck | Subacute to chronic neck pain | Underwent a neuroreflexotherapy intervention. | NRS in neck | 1.5 |
| NRS in arm | 1.5 | ||||||||
|
|
|||||||||
| Pool et al [44] | Netherlands | 2007 | Prospective cohort | ROC & anchor-based | Neck | Population with neck pain | Physiotherapy & manual therapy | NRS | 2.5 |
| NDI | 3.5 | ||||||||
|
|
|||||||||
| Vos et al [45] | Netherlands | 2006 | Prospective cohort | MDC | Neck | Acute neck pain (< 6 wk) | Physiotherapy consisting of manual therapy techniques | NDI | 1.66 |
|
|
|||||||||
| Childs et al [77] | USA | 2005 | Cohort | Anchor-based | Back | Low back pain | Physical therapy | NPRS | 2 |
|
|
|||||||||
| Davidson et al [78] | Australia | 2004 | Prospective cohort | Distribution-based, criterion-based, & 1 novel strategy | Back | Low back pain | Physiotherapy | SF-36 PF | 12 |
|
|
|||||||||
| Medication | |||||||||
|
|
|||||||||
| Bahadir et al [15] | Turkey | 2021 | Prospective cohort | Anchor-based | Back | Adult spine deformity | Pain medication | ODI | 2.23–14.31 |
| COMI | 0.27–2.62 | ||||||||
| 22-item Scoliosis Research Society Outcomes | 0.01–0.71 | ||||||||
|
|
|||||||||
| Exercise & education | |||||||||
|
|
|||||||||
| Maughan et al [18] | UK | 2010 | Prospective cohort | Anchor-based & distribution based | Back | Chronic low back pain | Exercise & education | NRS | 4 |
| RMDQ | 4 | ||||||||
| ODI | 8 | ||||||||
| PSEQ | 9 | ||||||||
| PSFS | 2 | ||||||||
|
|
|||||||||
| Spinal cord stimulation | |||||||||
|
|
|||||||||
| Sabourin et al [16] | USA | 2021 | Prospective cohort | Anchor-based | Back | Chronic pain | Spinal cord stimulation | MPQ | 1–2.3 |
| PCS | 1.9–13.6 | ||||||||
| NRS | 0.9–2.7 | ||||||||
| ODI | 3.5–6.9 | ||||||||
| BDI | 2–5.9 | ||||||||
|
|
|||||||||
| Goudman et al [64] | Belgium | 2021 | Prospective cohort | Anchor-based & distribution based | Back | Spinal pain | Spinal cord stimulation | Absolute change score from baseline up to 12 months of HD-SCS | 87.97 |
|
|
|||||||||
| Paul et al [17] | USA | 2017 | Prospective cohort | anchor-based | Back | Post laminectomy syndrome | Spinal cord stimulation | VAS | 1.2–3.7 |
| ODI | 8.2 | ||||||||
| BDI | 6.9 | ||||||||
|
|
|||||||||
| Acupuncture & Chuna (Tuina) | |||||||||
|
|
|||||||||
| Young et al[39] | USA | 2019 | Secondary analysis of an RCT | ROC & anchor-based | Neck | Neck pain with cervicogenic headaches | Thoracic manipulation mobilization & exercise | NRS | 2.5 |
| NDI | 5.5 | ||||||||
|
|
|||||||||
| Young et al [75] | USA | 2019 | Secondary analysis of an RCT | ROC & anchor-based | Neck | Neck pain without concomitant upper extremity symptoms | High velocity low-amplitude thrust manipulation or non-thrust mobilization to the upper cervical (C1-2) & upper thoracic (T1-2) spine | NRS | 1.5 |
| NDI | 5.5 | ||||||||
|
|
|||||||||
| Park et al [13] | Korea | 2017 | Prospective cohort | Distribution based | Back | FBSS | Integrative Korean medicine treatment | ODI | 9 |
| VAS LBP | 22.5 | ||||||||
| VAS Leg pain | 27.5 | ||||||||
| SF-36 PCS | 10.2 | ||||||||
| SF-36 MCS | 4 | ||||||||
| overall health scores of SF-36 | 8.9 | ||||||||
| ODI | 15* | ||||||||
| VAS LBP | 32.5* | ||||||||
| VAS Leg pain | 37* | ||||||||
| SF-36 PCS | 19.7* | ||||||||
| SF-36 MCS | 19.3* | ||||||||
| overall health scores of SF-36 | 21.1* | ||||||||
|
|
|||||||||
| Lauche et al [42] | Germany | 2013 | Secondary analysis of an RCT | ROC & anchor-based | Neck | Chronic neck pain | Cupping | VAS | 8 |
| NDI | 3 | ||||||||
| SF-36-BP | 10 | ||||||||
| SF-36-PCS | 2.6 | ||||||||
| VAS | 26.5* | ||||||||
| NDI | 8.4* | ||||||||
| SF-36-BP | 15.5 | ||||||||
| SF-36-PCS | 5.1 | ||||||||
|
|
|||||||||
| Pool et al [44] | Netherlands | 2007 | Prospective cohort | ROC & anchor-based | Neck | Population with neck pain | Physiotherapy & manual therapy | NRS | 2.5 |
| NDI | 3.5 | ||||||||
|
|
|||||||||
| Vos et al [45] | Netherlands | 2006 | Prospective cohort | MDC | Neck | Acute neck pain (< 6 wk) | Physiotherapy consisting of manual therapy techniques | NDI | 1.66 |
|
|
|||||||||
| Rehabilitation program | |||||||||
|
|
|||||||||
| Monticone et al [83] | Italy | 2017 | Prospective cohort | Anchor & distribution based | Back | Rehabilitation after lumbar fusion | Motor & cognitive rehabilitation program | TSK | 6 |
| Harm & Activity Avoidance subscales | 4 | ||||||||
|
|
|||||||||
| Nonsurgical treatment | |||||||||
|
|
|||||||||
| Yuksel et al [19] | Turkey | 2019 | Prospective cohort | Anchor-based | Back | Adult spinal deformity | Nonsurgical treatment | COMI | 1.2 |
| ODI | 2.45 | ||||||||
| SF-36 PCS | 2.15 | ||||||||
| SF-36 MCS | 5.14 | ||||||||
| SRS-22R | 0.11 | ||||||||
|
|
|||||||||
| Hung et al [5] | USA | 2018 | Prospective cohort | Anchor-based & distribution-based | Spine | Spinal disorder | Nonsurgical & surgical treatment | PROMIS-PF | 8 |
| PROMIS-PI | 8 | ||||||||
| ODI | 24 | ||||||||
| NDI | 18 | ||||||||
* Substantial Clinical Benefit values.
COMI = Core Outcome Measures Index; EQ VAS = EuroQol Visual Analogue Scale; EQ-5D = European Quality of Life 5-Dimension; EQ-5D-3L = 3-Level European Quality of Life 5-Dimension; HD-SCS = High Density Spinal Cord Stimulation; JOA = Japanese Orthopaedic Association; JOABPEQ = Japanese Orthopedic Association Back Pain Evaluation Questionnaire; JOABPEQ-LBP = Japanese Orthopedic Association Back Pain Evaluation Questionnaire for Low Back Pain; JOACEMQ = Japanese Orthopaedic Association Cervical Myelopathy Evaluation Questionnaire; mJOA = modified Japanese Association Scale; MPQ = McGill Pain Questionnaire; NDI = Neck disability index; NPRS = Numeric pain rating scale; NRS = Numeric Rating Scale; NRS AP = Numeric Rating Scale for Arm Pain; NRS BP = Numeric Rating Scale for Back Pain; NRS LN = Numeric Rating Scale for leg numbness; NRS LP = Numeric Rating Scale for Leg Pain; NRS NP = Numeric Rating Scale for Neck Pain; ODI = Oswestry Disability Index; PHQ-9 = Patient Health Questionnaire-9; PRO-JOA = Patient-Reported Japanese Orthopaedic Association; PROMIS = Patient-Reported Outcomes Measurement Information System; PROMIS-PF = Patient-Reported Outcomes Measurement Information System-Physical Function; PSEQ = Pain Self-Efficacy Questionnaire; PSFS = Patient-Specific Functional Scale; QOL = Quality of life; RMDQ = Roland Morris Disability Questionnaire; SF-12 MCS = Short-Form 12-Item Health Survey Mental Component Score; SF-12 PCS = Short-Form 12-Item physical component survey; SF-36 = Short-Form 36-Item Health Survey; SF-36 MCS = Short-Form 36-Item Health Survey Mental Component Score; SF-36 PCS = Short-Form 36-Item physical component survey; SF-36 PF = Short Form 36-item Health Survey for physical function; SF-36-BP = short-form 36 health survey for bodily pain; SF-8 MCS = Short-Form 8-Item Health Survey Mental Component Score; SF-8 PCS = Short-Form 8-Item physical component score; SRS = Session Rating Scale; SRS-22 = Scoliosis Research Society-22; TSK = Tampa Scale of Kinesiophobia; TUG = Timed Up and Go Test; VAS = Visual Analogue Scale; VAS AP = Visual Analogue Scale for Arm Pain; VAS LBP = Visual Analogue Scale for Low Back Pain; VAS NP = Visual Analogue Scale for Neck Pain; VAS AP = Visual Analogue Scale for Arm Pain; VAS BP = Visual Analogue Scale for Back Pain; VAS LP = Visual Analogue Scale for Leg Pain; VR-12 MCS = Veterans RAND 12-Item Health Survey Mental Component Score; VR-12 PCS = Veterans RAND 12-Item Health Survey for Physical Component Score; ZCQ = Zurich Claudication Questionnaire; ZDS = Zagazig Depression Scale.
| Authors [ref] | Design | Method | Region | Disease | Intervention | Reported MCID |
|---|---|---|---|---|---|---|
| Non-surgical | ||||||
|
|
||||||
| Bahadir et al [15] | Prospective cohort | Anchor-based | Back | Adult spine deformity | Pain medication | 2.23–14.31 |
|
|
||||||
| Sabourin et al [16] | Prospective cohort | Anchor-based | Back | Chronic pain | Spinal cord stimulation | 3.5–6.9 |
|
|
||||||
| Yuksel et al [19] | Prospective cohort | Anchor-based | Back | Adult spine deformity | Nonsurgical treatment | 2.45 |
|
|
||||||
| Hung et al [5] | Prospective cohort | Anchor-based & distribution based | Spine | Spine disorder | Nonsurgical treatment | 24 |
|
|
||||||
| Paul et al [17] | Prospective cohort | Anchor-based | Back | Post laminectomy syndrome | Spinal cord stimulation | 8.2 |
|
|
||||||
| Park et al [13] | Prospective cohort | Distribution based | Back | FBSS | Integrative Korean medicine treatment | 9 |
|
|
||||||
| Maughan et al [18] | Prospective cohort | Anchor-based & distribution based | Back | Chronic low back pain | Exercise & education | 8 |
|
|
||||||
| Fritz et al [20] | Prospective cohort | Anchor-based | Back | Low back pain | Physical therapy | 50% |
|
|
||||||
| Surgical | ||||||
|
|
||||||
| Nakarai et al [22] | Retrospective cohort | Anchor-based | Back | Lumbar spinal stenosis | Decompression surgery | 42.40% |
|
|
||||||
| Shahi et al [21] | Retrospective review of prospectively collected data | Anchor-based | Back | Degenerative lumbar spine pathology | Minimally invasive transforaminal lumbar interbody fusion or decompression surgery | 25.2 |
|
|
||||||
| Vanhorn et al [23] | Retrospective chart review | Anchor-based | Back | Lumbar spinal stenosis | Lumbar tubular micro decompression surgery | 15.0–16.5 |
|
|
||||||
| Bahadir et al [15] | Prospective cohort | Anchor-based | Back | Adult spine deformity | Fusion decompression surgery | 2.23–14.31 |
|
|
||||||
| Lewandrowski et al [24] | Retrospective cohort | Anchor-based | Back | Lumbar spinal stenosis | Transforaminal endoscopic lumbar decompression surgery | 15–16.5 |
|
|
||||||
| Laratta et al [25] | Retrospective cohort | Anchor & distribution based | Back |
Grade 1 degenerative spondylolisthesis + obesity Grade 1 degenerative spondylolisthesis Grade 1 degenerative spondylolisthesis + anxiety Grade 1 degenerative spondylolisthesis + depression |
Lumbar fusion surgery | 20.58 |
| 20.69 | ||||||
| 24.72 | ||||||
| 22.56 | ||||||
|
|
||||||
| Yoshida et al [26] | Retrospective cohort | Anchor-based | Back | Adult spinal deformity | Deformity surgery | 11% |
|
|
||||||
| Yuksel et al [19] | Prospective cohort | Anchor-based | Back | Adult spine deformity | Surgical treatment | 14.96 |
|
|
||||||
| Austevoll et al [27] | Retrospective chart review | Anchor-based | Back | Lumbar spinal stenosis & Lumbar degenerative spondylolisthesis | Decompression & fusion | 24 |
| 30% | ||||||
|
|
||||||
| Asher et al [14] | Prospective cohort | Anchor-based | Back | Lumbar degenerative spondylolisthesis | Fusion surgery & laminectomy | 26.6 |
| Distribution based | 14.3 | |||||
|
|
||||||
| Patel et al [28] | Retrospective cohort | Anchor-based | Back | Lumbar degenerative disc disease | Discectomy | 12 |
| Anchor-based | Decompression surgery | 10 | ||||
| ROC analysis | Fusion surgery | 12.5 | ||||
|
|
||||||
| Solberg et al [29] | Prospective cohort | Anchor-based | Back | Lumbar disc herniation | Discectomy | 20 |
|
|
||||||
| Gum et al [30] | Prospective cohort | Anchor & distribution based | Back | Spondylolisthesis, stenosis, disc pathology, scoliosis, & spine instability | Fusion surgery | 0.17–9.06 |
|
|
||||||
| Carreon et al [31] | Prospective cohort | Distribution based | Back | Lumbar degenerative disorders | Fusion surgery | 12.4 |
|
|
||||||
| Parker et al [32] | Prospective cohort | Anchor-based | Back | Same-level recurrent lumbar stenosis | Neural decompression & fusion surgery | 8.2 |
|
|
||||||
| Parker et al [33] | Prospective cohort | Anchor-based | Back | Lumbar adjacent-segment disease | Fusion surgery | 6.8–16.9 |
|
|
||||||
| Parker et al [34] | Prospective cohort | Anchor-based | Back | Symptomatic pseudoarthrosis | Revision fusion surgery | 8.6 |
|
|
||||||
| Parker et al [35] | Prospective cohort | Anchor-based | Back | Degenerative lumbar spondylolisthesis | Transforaminal lumbar interbody fusion surgery | 11–22.9 |
|
|
||||||
| Copay et al [36] | Retrospective chart review | Anchor & distribution based | Back | Spinal stenosis, lumbar disc pathology/degeneration, spondylolisthesis | Fusion surgery & decompression surgery | 12.8 |
|
|
||||||
| Tafazal et al [37] | Prospective cohort | Anchor-based | Back | Various spine disorders | Discectomy | 27 |
| Decompression surgery | 16 | |||||
| Fusion surgery | 13 | |||||
| Authors [ref] | Design | Method | Region | Disease | Intervention | Reported MCID |
|---|---|---|---|---|---|---|
| Non-Surgical | ||||||
| Young et al [39] | Secondary analysis of a RCT | ROC & anchor-based | Neck | Neck pain with cervicogenic headaches | Thoracic manipulation mobilization & exercise. | 3.5 – 5.5 |
| Young et al [75] | Secondary analysis of a RCT | ROC & anchor-based | Neck | Neck pain without concomitant upper extremity symptoms | High velocity low-amplitude thrust manipulation or non-thrust mobilization to the upper cervical (C1-2) & upper thoracic (T1-2) spine. | 5.5 |
| Hung et al [5] | Prospective cohort | Anchor-based & distribution based | Spine | Spine disorder | Nonsurgical treatment | 18 |
| Jørgensen et al [40] | Secondary analysis of an RCT | Anchor-based | Neck | Chronic neck pain | Physical training | 20–60% |
| Pereira et al [41] | Prospective cohort | Anchor-based | Neck | Chronic neck pain | Physical therapy | 5.5 |
| Lauche et al [42] | Secondary analysis of an RCT | ROC & anchor-based | Neck | Chronic neck pain | Cupping | 3 |
| Young et al [75] | Prospective cohort | Anchor-based | Neck | Mechanical neck disorders | Physical therapy | 7.5 |
| Cleland et al [43] | Prospective cohort | ROC & anchor-based | Neck | Neck pain | Underwent 1 PT treatment session consisting of manual therapy. | 19% |
| Vos et al [45] | Prospective cohort | MDC | Neck | Acute neck pain (< 6 wk) | Physiotherapy consisting of manual therapy techniques. | 1.66 |
| Pool et al [44] | Prospective cohort | ROC & anchor-based | Neck | Population with neck pain | Physiotherapy & manual therapy | 3.5 |
| Surgical | ||||||
| Mjåset et al [46] | Prospective cohort | Anchor-based | Neck | Degenerative cervical myelopathy | ACDF | 16% |
| Khan et al [47] | Retrospective chart review | Anchor-based | Neck | Degenerative cervical disease | ACDF | 30% |
| Soroceaunu et al [48] | Prospective cohort | Anchor & distribution based | Neck | Adult cervical deformity | Deformity surgery | 7 |
| Kato et al [50] | Retrospective chart review | Anchor & distribution based | Neck | Degenerative cervical myelopathy | Laminoplasty | 4.2 |
| Steinhaus et al [49] | Prospective cohort | Anchor & distribution based | Neck | Cervical spine pathology (myelopathy, radiculopathy, myeloradiculopathy) | Cervical spine surgery | 8.5 |
| Parker et al [52] | Prospective cohort | Anchor-based | Neck | Cervical radiculopathy | ACDF & discectomy | 17.3% |
| Auffinger et al [72] | Prospective cohort | Anchor & distribution based | Neck | Subaxial degenerative cervical spine disease | Fusion surgery | 2.72–12.08 |
| Carreon et al [53] | Prospective cohort | Anchor & distribution based | Neck | Degenerative cervical spine disorder | Fusion surgery | 7.5 |
- [1] Jaeschke R, Singer J, Guyatt GH. Measurement of health status. Ascertaining the minimal clinically important difference. Control Clin Trials 1989;10(4):407−15.PubMed
- [2] Beaton DE, Boers M, Wells GA. Many faces of the minimal clinically important difference (MCID): a literature review and directions for future research. Curr Opin Rheumatol 2002;14(2):109−14.ArticlePubMed
- [3] Chung AS, Copay AG, Olmscheid N, Campbell D, Walker JB, Chutkan N. Minimum Clinically Important Difference: Current Trends in the Spine Literature. Spine (Phila Pa 1976) 2017;42(14):1096−105.PubMed
- [4] Kolin DA, Moverman MA, Pagani NR, Puzzitiello RN, Dubin J, Menendez ME, et al. Substantial Inconsistency and Variability Exists Among Minimum Clinically Important Differences for Shoulder Arthroplasty Outcomes: A Systematic Review. Clin Orthop Relat Res 2022;480(7):1371−83.ArticlePubMedPMC
- [5] Hung M, Saltzman CL, Kendall R, Bounsanga J, Voss MW, Lawrence B, et al. What Are the MCIDs for PROMIS, NDI, and ODI Instruments Among Patients With Spinal Conditions? Clin Orthop Relat Res 2018;476(10):2027−36.ArticlePubMedPMC
- [6] Yuksel S, Ayhan S, Nabiyev V, Domingo-Sabat M, Vila-Casademunt A, Obeid I, et al. Minimum clinically important difference of the health-related quality of life scales in adult spinal deformity calculated by latent class analysis: is it appropriate to use the same values for surgical and nonsurgical patients? Spine J 2019;19(1):71−8.ArticlePubMed
- [7] Colquhoun HL, Levac D, O’Brien KK, Straus S, Tricco AC, Perrier L, et al. Scoping reviews: time for clarity in definition, methods, and reporting. J Clin Epidemiol 2014;67(12):1291−4.ArticlePubMed
- [8] Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med 2018;169(7):467−73.ArticlePubMed
- [9] Peters MDJGC, McInerney P, Munn Z, Tricco AC, Khalil H. JBI Manual for Evidence Synthesis. Joanna Briggs Institute, 2020.
- [10] Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8(1):19−32.Article
- [11] Maldaner N, Sosnova M, Ziga M, Zeitlberger AM, Bozinov O, Gautschi OP, et al. External Validation of the Minimum Clinically Important Difference in the Timed-up-and-go Test After Surgery for Lumbar Degenerative Disc Disease. Spine (Phila Pa 1976) 2022;47(4):337−42.ArticlePubMed
- [12] Gautschi OP, Stienen MN, Corniola MV, Joswig H, Schaller K, Hildebrandt G, et al. Assessment of the Minimum Clinically Important Difference in the Timed Up and Go Test After Surgery for Lumbar Degenerative Disc Disease. Neurosurgery 2017;80(3):380−5.ArticlePubMedPDF
- [13] Park KB, Shin JS, Lee J, Lee YJ, Kim MR, Lee JH, et al. Minimum Clinically Important Difference and Substantial Clinical Benefit in Pain, Functional, and Quality of Life Scales in Failed Back Surgery Syndrome Patients. Spine (Phila Pa 1976) 2017;42(8):E474−81.ArticlePubMed
- [14] Asher AL, Kerezoudis P, Mummaneni PV, Bisson EF, Glassman SD, Foley KT, et al. Defining the minimum clinically important difference for grade I degenerative lumbar spondylolisthesis: insights from the Quality Outcomes Database. Neurosurg Focus 2018;44(1):E2. Article
- [15] Bahadır S, Yuksel S, Ayhan S, Nabi V, Vila-Casademunt A, Obeid I, et al. Variation of Minimum Clinically Important Difference by Age, Gender, Baseline Disability, and Change of Direction in Adult Spinal Deformity Population: Is It a Constant Value? World Neurosurg 2021;146:e1171−6.ArticlePubMed
- [16] Sabourin S, Tram J, Sheldon BL, Pilitsis JG. Defining minimal clinically important differences in pain and disability outcomes of patients with chronic pain treated with spinal cord stimulation. J Neurosurg Spine 2021;35(2):243−50.ArticlePubMed
- [17] Paul AR, Kumar V, Roth S, Gooch MR, Pilitsis JG. Establishing Minimal Clinically Important Difference of Spinal Cord Stimulation Therapy in Post-Laminectomy Syndrome. Neurosurgery 2017;81(6):1011−5.ArticlePubMedPDF
- [18] Maughan EF, Lewis JS. Outcome measures in chronic low back pain. Eur Spine J 2010;19(9):1484−94.ArticlePubMedPMCPDF
- [19] Yuksel S, Ayhan S, Nabiyev V, Domingo-Sabat M, Vila-Casademunt A, Obeid I, et al. Minimum clinically important difference of the health-related quality of life scales in adult spinal deformity calculated by latent class analysis: is it appropriate to use the same values for surgical and nonsurgical patients? Spine J 2019;19(1):71−8.ArticlePubMed
- [20] Fritz JM, Hebert J, Koppenhaver S, Parent E. Beyond minimally important change: defining a successful outcome of physical therapy for patients with low back pain. Spine (Phila Pa 1976) 2009;34(25):2803−9.PubMed
- [21] Shahi P, Shinn D, Singh N, Subramanian T, Song J, Dalal S, et al. ODI <25 Denotes Patient Acceptable Symptom State After Minimally Invasive Lumbar Spine Surgery. Spine (Phila Pa 1976) 2023;48(3):196−202.ArticlePubMed
- [22] Nakarai H, Kato S, Kawamura N, Higashikawa A, Takeshita Y, Fukushima M, et al. Minimal clinically important difference in patients who underwent decompression alone for lumbar degenerative disease. Spine J 2022;22(4):549−60.ArticlePubMed
- [23] Vanhorn TA, Knio ZO, O’Gara TJ. Defining a Minimum Clinically Important Difference in Patient-Reported Outcome Measures in Lumbar Tubular Microdecompression Patients. Int J Spine Surg 2020;14(4):538−43.ArticlePubMedPMC
- [24] Lewandrowski KU, PSTDEC , PDEC , Yeung A. Minimal Clinically Important Difference in Patient-Reported Outcome Measures with the Transforaminal Endoscopic Decompression for Lateral Recess and Foraminal Stenosis. Int J Spine Surg 2020;14(2):254−66.ArticlePubMedPMC
- [25] Laratta J, Carreon LY, Buchholz AL, Yew AY, Bisson EF, Mummaneni PV, et al. Effects of preoperative obesity and psychiatric comorbidities on minimum clinically important differences for lumbar fusion in grade 1 degenerative spondylolisthesis: analysis from the prospective Quality Outcomes Database registry. J Neurosurg Spine 2020;33(5):635−42.ArticlePubMed
- [26] Yoshida G, Hasegawa T, Yamato Y, Kobayashi S, Shin O, Banno T, et al. Minimum Clinically Important Differences in Oswestry Disability Index Domains and Their Impact on Adult Spinal Deformity Surgery. Asian Spine J 2019;13(1):35−44.ArticlePubMedPMCPDF
- [27] Austevoll IM, Gjestad R, Grotle M, Solberg T, Brox JI, Hermansen E, et al. Follow-up score, change score or percentage change score for determining clinical important outcome following surgery? An observational study from the Norwegian registry for Spine surgery evaluating patient reported outcome measures in lumbar spinal stenosis and lumbar degenerative spondylolisthesis. BMC Musculoskelet Disord 2019;20(1):31. ArticlePubMedPMCPDF
- [28] Patel MS, Newey M, Sell P. A comparison of patient-reported outcome measures after spinal surgery. Bone Joint J 2015;97-B(3):366−71.ArticlePubMedPDF
- [29] Solberg T, Johnsen LG, Nygaard ØP, Grotle M. Can we define success criteria for lumbar disc surgery?: estimates for a substantial amount of improvement in core outcome measures. Acta Orthop 2013;84(2):196−201.PubMedPMC
- [30] Gum JL, Glassman SD, Carreon LY. Clinically important deterioration in patients undergoing lumbar spine surgery: a choice of evaluation methods using the Oswestry Disability Index, 36-Item Short Form Health Survey, and pain scales: clinical article. J Neurosurg Spine 2013;19(5):564−8.PubMed
- [31] Carreon LY, Bratcher KR, Canan CE, Burke LO, Djurasovic M, Glassman SD. Differentiating minimum clinically important difference for primary and revision lumbar fusion surgeries. J Neurosurg Spine 2013;18(1):102−6.ArticlePubMed
- [32] Parker SL, Mendenhall SK, Shau DN, Adogwa O, Anderson WN, Devin CJ, et al. Minimum clinically important difference in pain, disability, and quality of life after neural decompression and fusion for same-level recurrent lumbar stenosis: understanding clinical versus statistical significance. J Neurosurg Spine 2012;16(5):471−8.ArticlePubMed
- [33] Parker SL, Mendenhall SK, Shau D, Adogwa O, Cheng JS, Anderson WN, et al. Determination of minimum clinically important difference in pain, disability, and quality of life after extension of fusion for adjacent-segment disease. J Neurosurg Spine 2012;16(1):61−7.ArticlePubMed
- [34] Parker SL, Adogwa O, Mendenhall SK, Shau DN, Anderson WN, Cheng JS, et al. Determination of minimum clinically important difference (MCID) in pain, disability, and quality of life after revision fusion for symptomatic pseudoarthrosis. Spine J 2012;12(12):1122−8.ArticlePubMed
- [35] Parker SL, Adogwa O, Paul AR, Anderson WN, Aaronson O, Cheng JS, et al. Utility of minimum clinically important difference in assessing pain, disability, and health state after transforaminal lumbar interbody fusion for degenerative lumbar spondylolisthesis. J Neurosurg Spine 2011;14(5):598−604.ArticlePubMed
- [36] Copay AG, Glassman SD, Subach BR, Berven S, Schuler TC, Carreon LY. Minimum clinically important difference in lumbar spine surgery patients: a choice of methods using the Oswestry Disability Index, Medical Outcomes Study questionnaire Short Form 36, and pain scales. Spine J 2008;8(6):968−74.ArticlePubMed
- [37] Tafazal SI, Sell PJ. Outcome scores in spinal surgery quantified: excellent, good, fair and poor in terms of patient-completed tools. Eur Spine J 2006;15(11):1653−60.ArticlePubMedPDF
- [38] Young Ia PtD, Dunning JPtDPT, Butts RPtP, Mourad FPtDPT, Cleland Ja PtP. Reliability, construct validity, and responsiveness of the neck disability index and numeric pain rating scale in patients with mechanical neck pain without upper extremity symptoms. Physiother Theory Pract 2019;35(12):1328−35.ArticlePubMed
- [39] Young IA, Dunning J, Butts R, Cleland JA, Fernandez-de-Las-Penas C. Psychometric properties of the Numeric Pain Rating Scale and Neck Disability Index in patients with cervicogenic headache. Cephalalgia 2019;39(1):44−51.ArticlePubMedPDF
- [40] Jørgensen R, Ris I, Juhl C, Falla D, Juul-Kristensen B. Responsiveness of clinical tests for people with neck pain. BMC Musculoskelet Disord 2017;18(1):548. ArticlePubMedPMCPDF
- [41] Pereira M, Cruz EB, Domingues L, Duarte S, Carnide F, Fernandes R. Responsiveness and Interpretability of the Portuguese Version of the Neck Disability Index in Patients With Chronic Neck Pain Undergoing Physiotherapy. Spine (Phila Pa 1976) 2015;40(22):E1180−6.ArticlePubMed
- [42] Lauche R, Langhorst J, Dobos GJ, Cramer H. Clinically meaningful differences in pain, disability and quality of life for chronic nonspecific neck pain - a reanalysis of 4 randomized controlled trials of cupping therapy. Complement Ther Med 2013;21(4):342−7.ArticlePubMed
- [43] Cleland JA, Childs JD, Whitman JM. Psychometric properties of the Neck Disability Index and Numeric Pain Rating Scale in patients with mechanical neck pain. Arch Phys Med Rehabil 2008;89(1):69−74.ArticlePubMed
- [44] Pool JJ, Ostelo RW, Hoving JL, Bouter LM, de Vet HC. Minimal clinically important change of the Neck Disability Index and the Numerical Rating Scale for patients with neck pain. Spine (Phila Pa 1976) 2007;32(26):3047−51.ArticlePubMed
- [45] Vos CJ, Verhagen AP, Koes BW. Reliability and responsiveness of the Dutch version of the Neck Disability Index in patients with acute neck pain in general practice. Eur Spine J 2006;15(11):1729−36.ArticlePubMedPDF
- [46] Mjåset C, Zwart JA, Kolstad F, Solberg T, Grotle M. Clinical improvement after surgery for degenerative cervical myelopathy; A comparison of Patient-Reported Outcome Measures during 12-month follow-up. PLoS One 2022;17(3):e0264954. ArticlePubMedPMC
- [47] Khan I, Pennings JS, Devin CJ, Asher AM, Oleisky ER, Bydon M, et al. Clinically Meaningful Improvement Following Cervical Spine Surgery: 30% Reduction Versus Absolute Point-change MCID Values. Spine (Phila Pa 1976) 2021;46(11):717−25.ArticlePubMed
- [48] Soroceanu A, Smith JS, Lau D, Kelly MP, Passias PG, Protopsaltis TS, et al. Establishing the minimum clinically important difference in Neck Disability Index and modified Japanese Orthopaedic Association scores for adult cervical deformity. J Neurosurg Spine 2020;33(4):441−5.ArticlePubMed
- [49] Steinhaus ME, Iyer S, Lovecchio F, Khechen B, Stein D, Ross T, et al. Minimal Clinically Important Difference and Substantial Clinical Benefit Using PROMIS CAT in Cervical Spine Surgery. Clin Spine Surg 2019;32(9):392−7.ArticlePubMed
- [50] Kato S, Oshima Y, Matsubayashi Y, Taniguchi Y, Tanaka S, Takeshita K. Minimum clinically important difference in outcome scores among patients undergoing cervical laminoplasty. Eur Spine J 2019;28(5):1234−41.ArticlePubMedPDF
- [51] Auffinger B, Lam S, Shen J, Roitberg BZ. Measuring surgical outcomes in subaxial degenerative cervical spine disease patients: minimum clinically important difference as a tool for determining meaningful clinical improvement. Neurosurgery 2014;74(2):206−13. discussion 13-4.PubMed
- [52] Parker SL, Godil SS, Shau DN, Mendenhall SK, McGirt MJ. Assessment of the minimum clinically important difference in pain, disability, and quality of life after anterior cervical discectomy and fusion: clinical article. J Neurosurg Spine 2013;18(2):154−60.PubMed
- [53] Carreon LY, Glassman SD, Campbell MJ, Anderson PA. Neck Disability Index, short form-36 physical component summary, and pain scales for neck and arm pain: the minimum clinically important difference and substantial clinical benefit after cervical spine fusion. Spine J 2010;10(6):469−74.ArticlePubMed
- [54] Kovacs FM, Abraira V, Royuela A, Corcoll J, Alegre L, Tomas M, et al. Minimum detectable and minimal clinically important changes for pain in patients with nonspecific neck pain. BMC Musculoskelet Disord 2008;9:43. ArticlePubMedPMCPDF
- [55] MacDowall A, Skeppholm M, Robinson Y, Olerud C. Validation of the visual analog scale in the cervical spine. J Neurosurg Spine 2018;28(3):227−35.ArticlePubMed
- [56] Auffinger BM, Lall RR, Dahdaleh NS, Wong AP, Lam SK, Koski T, et al. Measuring surgical outcomes in cervical spondylotic myelopathy patients undergoing anterior cervical discectomy and fusion: assessment of minimum clinically important difference. PLoS One 2013;8(6):e67408. ArticlePubMedPMC
- [57] Ogura Y, Ogura K, Kobayashi Y, Kitagawa T, Yonezawa Y, Takahashi Y, et al. Minimum clinically important difference of major patient-reported outcome measures in patients undergoing decompression surgery for lumbar spinal stenosis. Clin Neurol Neurosurg 2020;196:105966. ArticlePubMed
- [58] Ogura Y, Ogura K, Kobayashi Y, Kitagawa T, Yonezawa Y, Takahashi Y, et al. Minimally clinically important differences for the Japanese Orthopaedic Association Back Pain Evaluation Questionnaire (JOABPEQ) following decompression surgery for lumbar spinal stenosis. J Clin Neurosci 2019;69:93−6.ArticlePubMed
- [59] Passias PG, Pierce KE, Williamson T, Naessig S, Ahmad W, Passfall L, et al. Establishing the minimal clinically important difference for the PROMIS. Physical domains in cervical deformity patients. J Clin Neurosci 2022;96:19−24.ArticlePubMed
- [60] Lynch CP, Cha EDK, Mohan S, Geoghegan CE, Jadczak CN, Singh K. Two-year validation and minimal clinically important difference of the Veterans RAND 12 Item Health Survey Physical Component Score in patients undergoing minimally invasive transforaminal lumbar interbody fusion. J Neurosurg Spine 2021;36(5):731−40.ArticlePubMed
- [61] Khutok K, Janwantanakul P, Jensen MP, Kanlayanaphotporn R. Responsiveness of the PROMIS-29 Scales in Individuals With Chronic Low Back Pain. Spine (Phila Pa 1976) 2021;46(2):107−13.ArticlePubMed
- [62] Joelson A, Nerelius F, Sigmundsson FG, Karlsson J. The minimal important change for the EQ VAS based on the SF-36 health transition item: observations from 25772 spine surgery procedures. Qual Life Res 2022;31(12):3459−66.ArticlePubMedPMCPDF
- [63] Zeitlberger AM, Sosnova M, Ziga M, Regli L, Bozinov O, Weyerbrock A, et al. Assessment of the Minimum Clinically Important Difference in the Smartphone-based 6-minute Walking Test After Surgery for Lumbar Degenerative Disc Disease. Spine (Phila Pa 1976) 2021;46(18):E959−65.ArticlePubMed
- [64] Goudman L, Billot M, Duarte RV, Eldabe S, Rigoard P, Moens M. Gradation of Clinical Holistic Response as New Composite Outcome to Evaluate Success in Spinal Cord Stimulation Studies for Pain. Neuromodulation 2023;26(1):139−46.ArticlePubMed
- [65] Fukushima M, Oka H, Oshima Y, Yuzawa Y, Matsudaira K, Tanaka S, et al. Evaluation of the Minimum Clinically Important Differences of the Zurich Claudication Questionnaire in Patients With Lumbar Spinal Stenosis. Clin Spine Surg 2020;33(10):E499−503.ArticlePubMed
- [66] Kato S, Oshima Y, Matsubayashi Y, Taniguchi Y, Tanaka S, Takeshita K. Minimum Clinically Important Difference and Patient Acceptable Symptom State of Japanese Orthopaedic Association Score in Degenerative Cervical Myelopathy Patients. Spine (Phila Pa 1976) 2019;44(10):691−7.ArticlePubMed
- [67] Berven S, Baron M, Deviren V, Glassman S, Bridwell K, Verma K. The Assessment of Clinically Significant Differences in Treating Spinal Deformity Using the SRS Questionnaire: What Is the Threshold of Change That Is Meaningful to Patients? Int J Spine Surg 2019;13(2):153−7.ArticlePubMedPMC
- [68] Carreon LY, Kelly MP, Crawford CH 3rd, Baldus CR, Glassman SD, Shaffrey CI, et al. SRS-22R Minimum Clinically Important Difference and Substantial Clinical Benefit After Adult Lumbar Scoliosis Surgery. Spine Deform 2018;6(1):79−83.ArticlePubMedPMC
- [69] Badhiwala JH, Witiw CD, Nassiri F, Akbar MA, Jaja B, Wilson JR, et al. Minimum Clinically Important Difference in SF-36 Scores for Use in Degenerative Cervical Myelopathy. Spine (Phila Pa 1976) 2018;43(21):E1260−6.ArticlePubMed
- [70] Azimi P, Yazdanian T, Benzel EC. Determination of minimally clinically important differences for JOABPEQ measure after discectomy in patients with lumbar disc herniation. J Spine Surg 2018;4(1):102−8.ArticlePubMedPMC
- [71] Tetreault L, Nouri A, Kopjar B, Côté P, Fehlings MG. The Minimum Clinically Important Difference of the Modified Japanese Orthopaedic Association Scale in Patients with Degenerative Cervical Myelopathy. Spine (Phila Pa 1976) 2015;40(21):1653−9.ArticlePubMed
- [72] Auffinger B, Lam S, Shen J, Thaci B, Roitberg BZ. Usefulness of minimum clinically important difference for assessing patients with subaxial degenerative cervical spine disease: statistical versus substantial clinical benefit. Acta Neurochir (Wien) 2013;155(12):2345−54. discussion 55.ArticlePubMedPDF
- [73] Skolasky RL, Albert TJ, Maggard AM, Riley LH 3rd. Minimum clinically important differences in the Cervical Spine Outcomes Questionnaire: results from a national multicenter study of patients treated with anterior cervical decompression and arthrodesis. J Bone Joint Surg Am 2011;93(14):1294−300.ArticlePubMed
- [74] Carreon LY, Sanders JO, Diab M, Sucato DJ, Sturm PF, Glassman SD. The minimum clinically important difference in Scoliosis Research Society-22 Appearance, Activity, And Pain domains after surgical correction of adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2010;35(23):2079−83.ArticlePubMed
- [75] Young BA, Walker MJ, Strunce JB, Boyles RE, Whitman JM, Childs JD. Responsiveness of the Neck Disability Index in patients with mechanical neck disorders. Spine J 2009;9(10):802−8.ArticlePubMed
- [76] Mannion AF, Porchet F, Kleinstück FS, Lattig F, Jeszenszky D, Bartanusz V, et al. The quality of spine surgery from the patient’s perspective: part 2. Minimal clinically important difference for improvement and deterioration as measured with the Core Outcome Measures Index. Eur Spine J 2009;18(Suppl 3):374−9.ArticlePubMedPMCPDF
- [77] Childs JD, Piva SR, Fritz JM. Responsiveness of the numeric pain rating scale in patients with low back pain. Spine (Phila Pa 1976) 2005;30(11):1331−4.ArticlePubMed
- [78] Davidson M, Keating JL, Eyres S. A low back-specific version of the SF-36 Physical Functioning scale. Spine (Phila Pa 1976) 2004;29(5):586−94.ArticlePubMed
- [79] Lynch CP, Cha EDK, Jenkins NW, Parrish JM, Mohan S, Jadczak CN, et al. The Minimum Clinically Important Difference for Patient Health Questionnaire-9 in Minimally Invasive Transforaminal Interbody Fusion. Spine (Phila Pa 1976) 2021;46(9):603−9.ArticlePubMed
- [80] Díaz-Arribas MJ, Fernández-Serrano M, Royuela A, Kovacs FM, Gallego-Izquierdo T, Ramos-Sánchez M, et al. Minimal Clinically Important Difference in Quality of Life for Patients With Low Back Pain. Spine (Phila Pa 1976) 2017;42(24):1908−16.ArticlePubMed
- [81] Takenaka H, Kamiya M, Sugiura H, Nishihama K, Ito A, Suzuki J, et al. Responsiveness and Minimal Clinically Important Difference of the 6-minute Walk Distance in Patients Undergoing Lumbar Spinal Canal Stenosis Surgery. Clin Spine Surg 2022;35(3):E345−50.ArticlePubMed
- [82] Zhou F, Zhang Y, Sun Y, Zhang F, Pan S, Liu Z. Assessment of the minimum clinically important difference in neurological function and quality of life after surgery in cervical spondylotic myelopathy patients: a prospective cohort study. Eur Spine J 2015;24(12):2918−23.ArticlePubMedPDF
- [83] Monticone M, Ambrosini E, Rocca B, Foti C, Ferrante S. Responsiveness and minimal clinically important changes for the Tampa Scale of Kinesiophobia after lumbar fusion during cognitive behavioral rehabilitation. Eur J Phys Rehabil Med 2017;53(3):351−8.ArticlePubMed
References
Figure & Data
References
Citations
- Minimum clinically important difference and substantial clinical benefit in patients with chronic temporomandibular disorders
Jaemin Son, Eun‐San Kim, Yoon Jae Lee, Nam‐Woo Lee, In‐Hyuk Ha
Journal of Oral Rehabilitation.2024;[Epub] CrossRef - Safety and effectiveness of integrative Korean medicine for the management of patients sustaining injuries in traffic accidents during pregnancy: A retrospective chart review and questionnaire survey
Dahyun Kyung, Kyoung Sun Park, Ji-Eun Koo, Sujin Kim, Jiwon Park, Jun-Hyo Bae, Jieun Bae, Suna Kim, Yoon Jae Lee, In-Hyuk Ha
Medicine.2024; 103(21): e38250. CrossRef



 PubReader
PubReader ePub Link
ePub Link Cite
Cite