Articles
- Page Path
- HOME > Perspect Integr Med > Volume 1(1); 2022 > Article
-
Original Article
An Overview of Clinical Features, and Medical Access Among Patients with Post-Acute COVID-19 Syndromes: Analysis of a Nationwide Survey in Korea -
Doori Kim1
 , Ui Min Jerng2
, Ui Min Jerng2 , Jee Young Lee3,*
, Jee Young Lee3,*
-
Perspectives on Integrative Medicine 2022;1(1):21-33.
DOI: https://doi.org/10.56986/pim.2022.09.005
Published online: September 30, 2022
1Department of Korean Medicine, Graduate School, Kyung Hee University, Seoul, Republic of Korea
2Department of Internal medicine, College of Korean Medicine, Sangji University, Wonju, Republic of Korea
3Department of Korean Internal Medicine, Integrative Cancer Center, Cha Ilsan Medical Center, Goyang, Republic of Korea
- *Corresponding author: Jee Young Lee, Department of Korean Internal Medicine, Integrative Cancer Center, Cha Ilsan Medical Center, 1205, Jungang-ro, Ilsandong-gu, Goyang, Gyeonggi-do, Republic of Korea, E-mail: happiade@daum.net
©2022 Jaseng Medical Foundation.
This is an open access article under the CC BY-NC license (http://creativecommons.org/licenses/by-nc/4.0/).
- 1,697 Views
- 45 Download
Abstract
-
Background
- The objective of this study was to identify the clinical features of patients who recovered from COVID-19, and to determine their unmet medical needs and quality of life.
-
Methods
- A cross-sectional national survey was conducted in Korea in June 2022, targeting patients with at least four weeks of symptoms of COVID-19. The questionnaire survey had 37 items across: basic characteristics, acute COVID-19 and post-acute COVID-19 syndrome (long COVID) symptoms, access to medical facilities for long COVID, unmet medical needs, long COVID support system, and quality of life.
-
Results
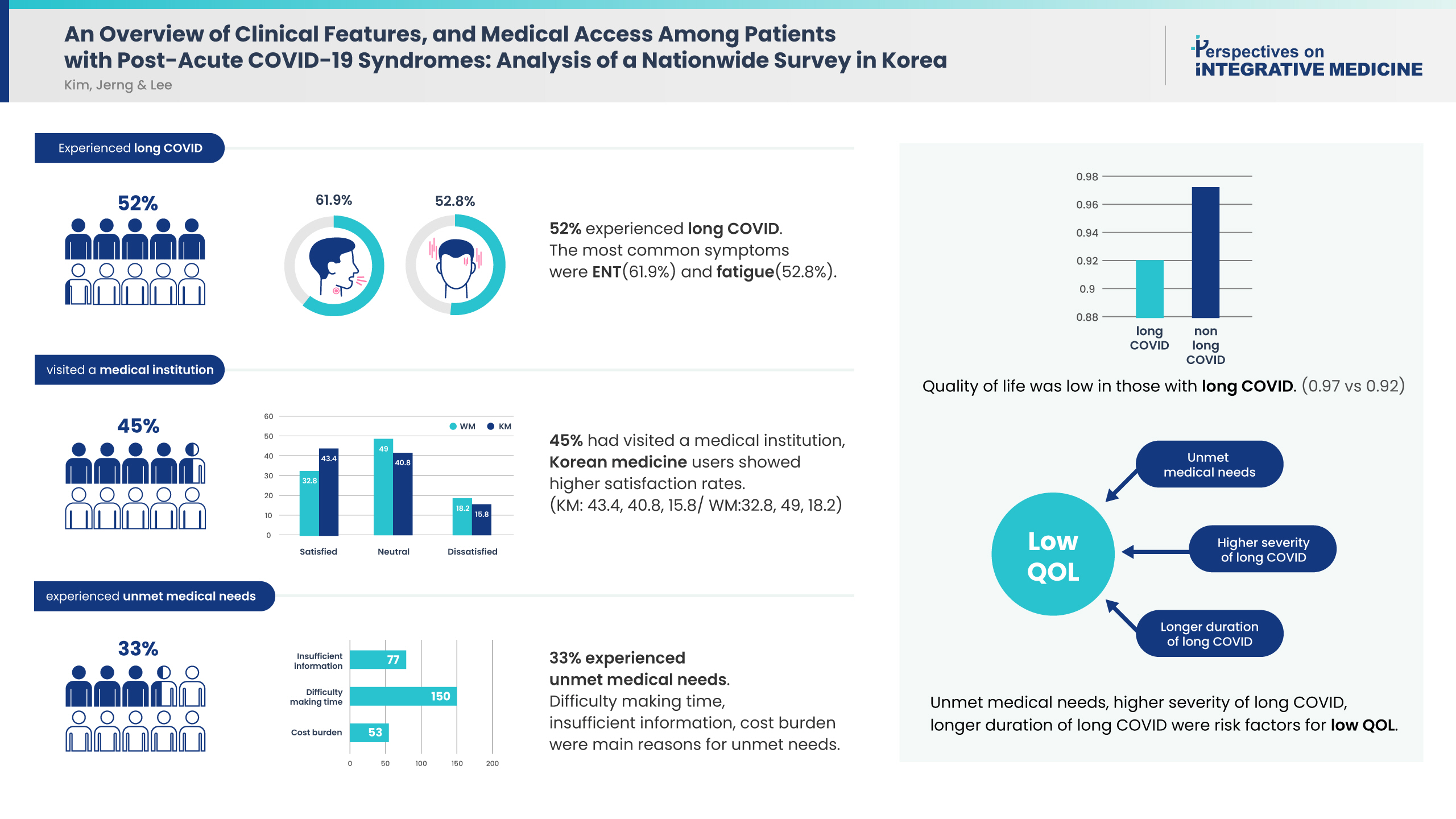
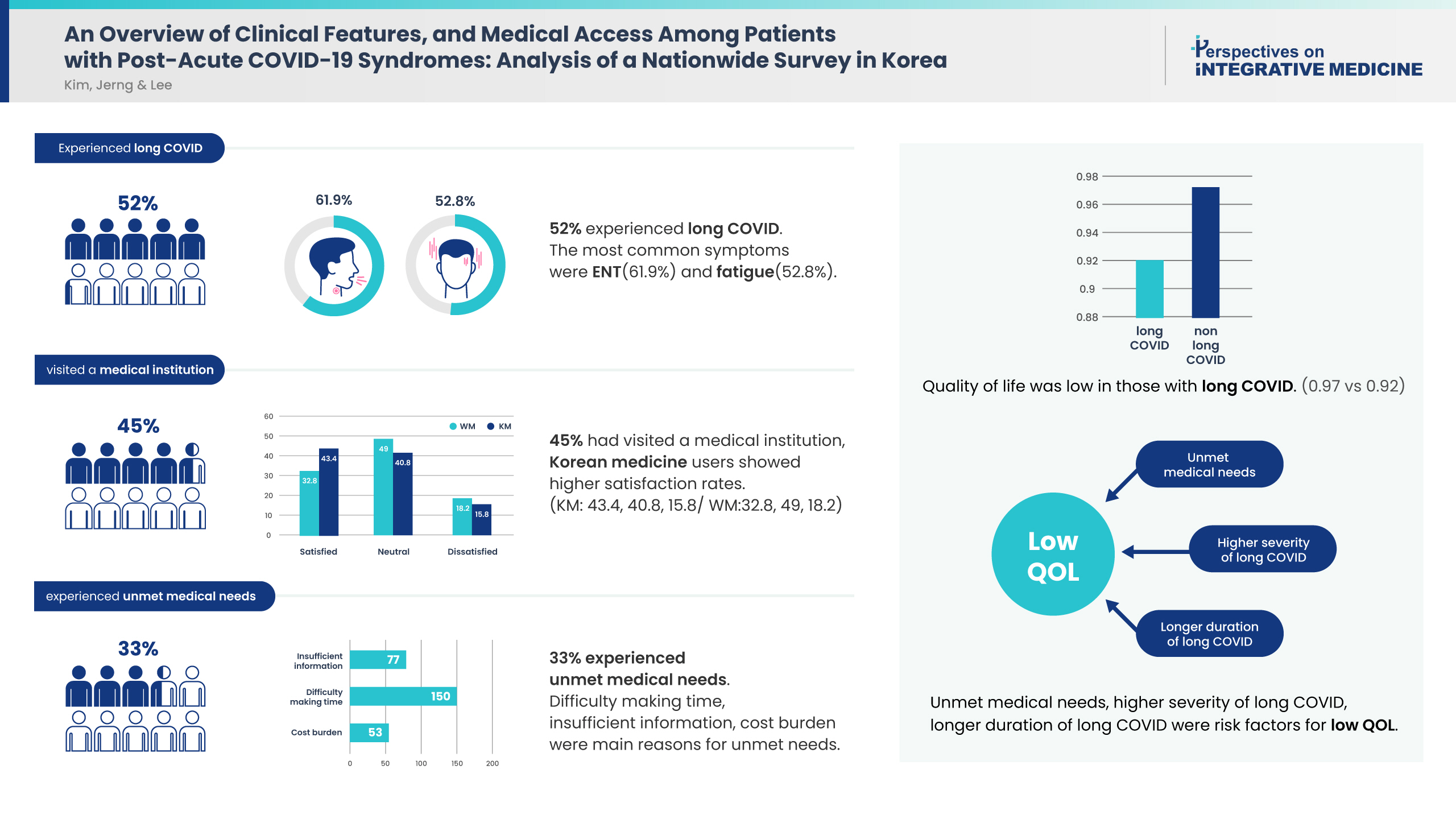
- Among 1,430 responses, 745 (52.1%) respondents had experienced long COVID. The most common symptoms were ear, nose, and throat complications (n = 461, 61.9%), followed by weakness and fatigue (n = 393, 52.8%). Amongst the 745 respondents who experienced long COVID, 337 (45.2%) had visited a medical institution, of which, 84.9% had visited a clinic or hospital for treatment. Korean medicine clinics and hospitals had the highest satisfaction rates (43.4%). There were 242 respondents (32.5%) who reported unmet medical needs for their long COVID. Symptom severity and duration of COVID-19 were risk factors for unmet medical needs. Quality of life was low in those patients with long COVID and unmet medical needs, and decreased further with increased severity and longer duration of symptoms.
-
Conclusion
- Studies on the effects of Korean medicine treatment of long COVID, and establishing a system providing sufficient treatment for patients with long COVID are needed. These findings could be used by clinicians, researchers, and COVID-19-related policymakers.
- Coronavirus disease 2019 (COVID-19) is caused by the severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) infection [1]. Due to rapid spread of the virus around the globe, 540 million confirmed cases of infection and over 6.3 million deaths had been reported worldwide by June 2022 [2]. In Korea, multiple waves of COVID-19 have occurred since the first confirmed case in January 2020, totaling over 18 million confirmed cases [2]. COVID-19 is characterized by a series of pulmonary and extrapulmonary symptoms, ranging from fever, upper respiratory symptoms, to gastrointestinal and musculoskeletal symptoms. While most recent cases are mild and some are asymptomatic, others may involve critical symptoms [1,3–6]; older patients and those with pre-existing conditions had a higher risk of severe COVID-19 [6–8].
- Most patients with mild infections recover from their symptoms within 2–4 weeks. However, some may continue to experience symptoms for more than a month [9,10]. The US Centers for Disease Control and Prevention stated that symptoms experienced four weeks after SARS-CoV-2 infection could be categorized as post-COVID conditions or long COVID [11]. In the following of this paper, we will use the commonly used ‘long COVID’, rather than the MESH term ‘post-acute COVID-19 syndrome’.
- Relatively few studies have focused on long COVID compared with acute COVID-19, but recent literature suggested that long COVID reportedly occur in 30–80% of infected patients [12–16]. SARS-CoV-2 affects multiple organ systems, and consequently, long COVID patients experience various systemic symptoms [17]. Typical long COVID symptoms include fatigue, dyspnea, dysgeusia or hyposmia, chest pain, coughing, and musculoskeletal pain [18,19].
- Long COVID also reduce the quality of life (QoL) [13,20,21]. In an Italian study of 143 patients who recovered from COVID-19, an assessment of QoL before and after COVID-19 using the EuroQol visual analog scale (EQ-VAS) revealed a decline in QoL in 44.1% of the patients [13]. In addition, a questionnaire survey conducted in Korea was conducted on 900 patients at least six months after SARS-CoV-2 infection which showed that 65% of the patients experienced long COVID, with fatigue being the most common sign [24]. Studies on patients after at least 12 months from SARS-CoV-2 infection [25,26] also revealed that nearly half of the patients still experienced long COVID. The most common were neuropsychiatric symptoms, such as cognitive impairment, anxiety, and depression. Such neuropsychiatric symptoms were also associated with a decline in QoL [25,26] which could also lead to impaired mobility [21] and further neuropsychiatric symptoms such sleep disturbance as well as activities of daily living such as self-care [22,23].
- Nearly 90% of all confirmed cases in Korea were reported in the three months between February and April 2022, when the spread of COVID-19 was rampant. COVID-19 cases from the later stages of the pandemic are different in many aspects from those that occurred in the early stages. New variants of SARS-CoV-2 have emerged over time, and new cases have shown increased infectivity of the virus and decreased severity in symptoms. While most patients who needed inpatient care gained access during the early stages of the pandemic, most patients during the latter stages of the pandemic received at-home treatment due to the lower severity of symptoms and shortage of hospital beds. Furthermore, the isolation period for individuals with COVID-19 was reduced to one week. However, studies on post-COVID have so far focused on patients who contracted COVID-19 at an early stage of the pandemic. In addition, still there is a high probability that patients with long COVID with inadequate treatments remain, considering the pandemic and the unmet medical needs due to avoidance and fear of crowded places and hospitals [27,28]. Moreover, policy support for these patients is yet unsufficient.
- To the best of our knowledge, no studies to date have investigated medical access and medical needs of long COVID patients, and none have assessed the clinical features with a focus on COVID-19 cases in 2022. The objective of this study was to identify the clinical features of patients who recovered from COVID-19, along with their medical access and unmet medical needs. The findings of the present study are expected to provide valuable data to clinicians treating long COVID patients, researchers, and COVID-19-related policymakers.
Introduction
- 1. Study design
- This cross-sectional national web-based questionnaire survey was conducted in Korea in June 2022. Survey data were collected using: (1) a mobile survey company; and (2) announcements on the Jaseng Medical Foundation (JMF) website. OpenSurvey is a mobile survey company with a registered panel of approximately 830,000 individuals categorized by sex, age, and region. Survey data from OpenSurvey and announcement of the website were collected between June 10 and June 13 and June 10 and 14, 2022, respectively.
- Prior to starting the survey, all participants were required to give their informed consent to participate in the study, and only those who provided consent were allowed to participate. The consent form included a brief introduction to the study, the inclusion criteria, and information regarding confidentiality. The survey was conducted anonymously, and personally identifiable information was encrypted before being relayed to the researchers. For confidentiality, access to raw data was restricted to the principal investigator and co-investigators with access to such data.
- The response data were managed by the principal investigator and co-investigators. To ensure the reliability of the questionnaire survey, incomplete questionnaires and those responses containing erroneous answers were excluded. Telephone numbers were used to identify and exclude duplicate participants.
- The study referred to the Checklist for Reporting of Survey Studies, and the study protocol and questionnaire were approved by the Institutional Review Board of Jaseng Hospital of Korean Medicine (approval no.: JASENG 2022-05-005; approval date: 20 May 2022).
- 2. Respondents
- The study targeted patients in whom symptoms of COVID-19 had lasted at least four weeks since their diagnosis. Based on reports of the numbers of COVID-19 patients experienced sequelae ranged from as much as 65% [24] and as little as 10% [29], a study population of more than 1,000 would be required to analyze at least 100 cases of sequelae of COVID-19. Assuming duplicates and an error response rate of 20%, the goal was to collect 1,500–2,000 responses.
- The inclusion criteria for the study were as follows: (1) patients diagnosed with COVID-19 at least four weeks prior to the survey; (2) adults aged 19–70 years; and (3) those who consented to participate in the questionnaire survey.
- 3. Survey
- The questionnaire was developed by reviewing previous studies and several rounds of internal discussion amongst researchers. The questionnaire consisted of 38 items divided into seven parts and required approximately eight minutes to complete. Details of the questionnaire were presented separately (Supplementary 1).
- 4. Statistical analysis
- Basic characteristics were expressed as mean ± SD for continuous variables and frequency (%) for categorical variables, depending on the presence/absence of long COVID. Differences in the percentage of basic characteristic variables, according to long COVID, were tested using the chi-square test or Fisher’s exact test. For continuous variables, differences, according to long COVID conditions, were tested using an independent t test. Survey items were expressed as mean ± SD for continuous variables and frequency (%) for categorical variables according to sex and age. Differences in percentages by sex and age were tested using the chi-square test or Fisher’s exact test. A logistic regression model was used to analyze the determinants of unmet medical needs. Univariate analysis was performed for each basic characteristic, COVID-19 severity, COVID-19 symptoms, and long COVID, after which multivariate analysis was performed using a model constructed based on the results of the univariate analysis. Each estimate was expressed as an odds ratio (OR) and 95% confidence interval (CI). Missing values were analyzed without imputation. All analyses were performed using the SAS software (Version 9.4; SAS Institute, Cary, NC, USA). Statistical significance was set at p < 0.05.
Materials and Methods
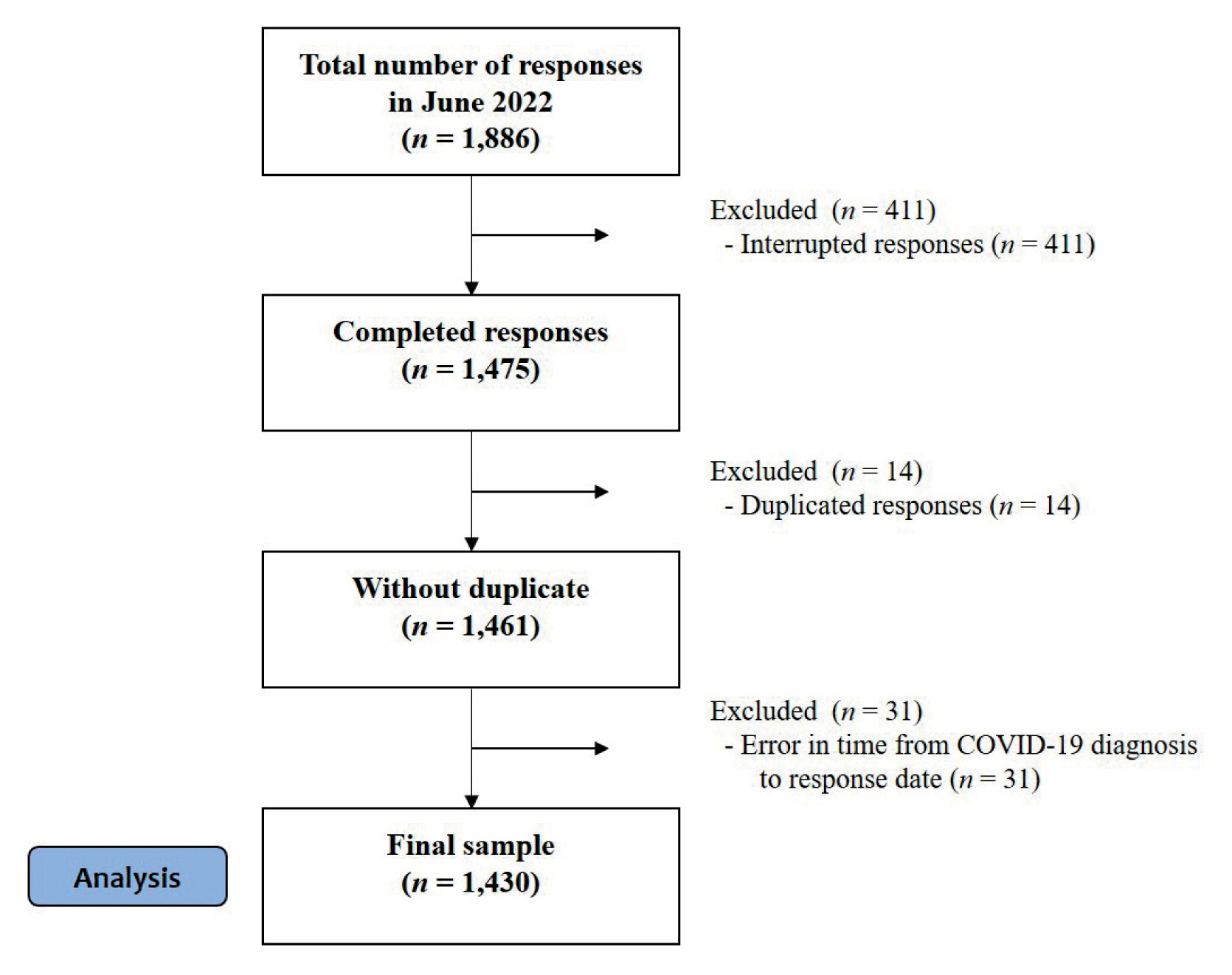
- 1. Basic characteristics of respondents
- A total of 1,886 responses were collected through OpenSurvey and its website. Of these, 411 incomplete questionnaires and 14 duplicates were excluded from the study. For duplicates, the most recent version was chosen. However, if there was a significant discrepancy in the sincerity of responses, the one with the more sincere responses was chosen. Moreover, 31 sets with clinical errors in responses were also excluded. Questionnaires that were complete from missing demographic information were included in the analysis. Ultimately, 1,430 sets of responses were included in the analysis (Fig. 1).
- Basic characteristics of the respondents according to long COVID is shown in Table 1. Amongst the 1,430 respondents, 745 (52.10%) stated that they had experienced post-COVID symptoms. There were 850 females (59.4%), which was significantly higher than males with long COVID (p < 0.0001). The mean age of the respondents was 38.20 ± 11.60 years, but the long COVID group had a higher mean age (p = 0.0192) and a higher percentage of older individuals (p = 0.0037). Moreover, the long COVID group had a higher percentage of patients with comorbidities (p = 0.0026). The acute COVID-19 symptoms experienced by the respondents included ENT symptoms (n = 1,201, 84.0%), fever (n = 876, 61.3%), weakness and fatigue (n = 852, 59.6%), and pain (n = 730, 61.3%). Most were mild cases that could be managed at home. The EuroQol-5 dimension (EQ-5D) score of the long COVID group was 0.92 ± 0.11 points, representing a significantly lower QoL compared with the respondents who had not developed post-COVID (p < 0.0001).
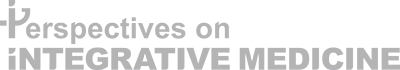
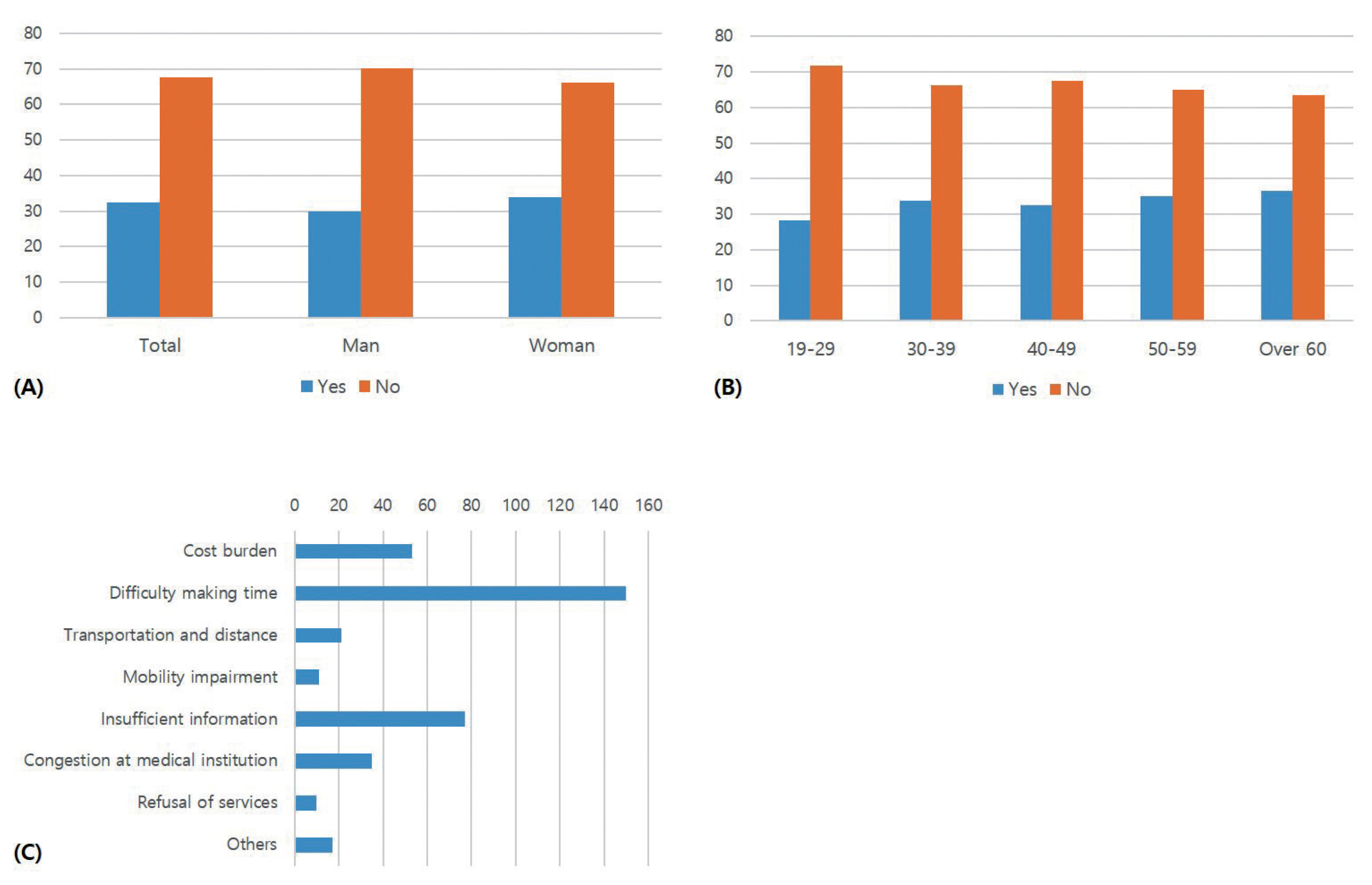
- 2. Symptoms and severity of long COVID
- The most common long COVID symptoms were ENT symptoms such as coughing, sputum, sore throat, and runny nose (n = 461, 61.9%), followed by weakness and fatigue (n = 393, 52.8%), and dysgeusia or hyposmia (n = 173, 23.2%). For all symptoms, there was a higher percentage of symptoms amongst females. The age group with the highest percentage of respondents with symptoms was in the age group ≥ 60 years (n = 24, 38.1%). The most severe symptoms were ENT (n = 338, 45.4%), followed by weakness (n = 208, 27.9%; Fig. 2, Supplementary Table 1).
- Approximately half of the respondents indicated mild to moderate severity symptoms. The percentage of women with more severe symptoms was higher (p = 0.0030; Table 2). Long COVID most often continued from diagnosis rather than new symptoms occurring (n = 453, 60.8%). Regarding the duration of long COVID, the most common response was 1–3 months (n = 329, 44.2%), followed by 2 weeks to a month (n = 236, 31.7; Table 2).
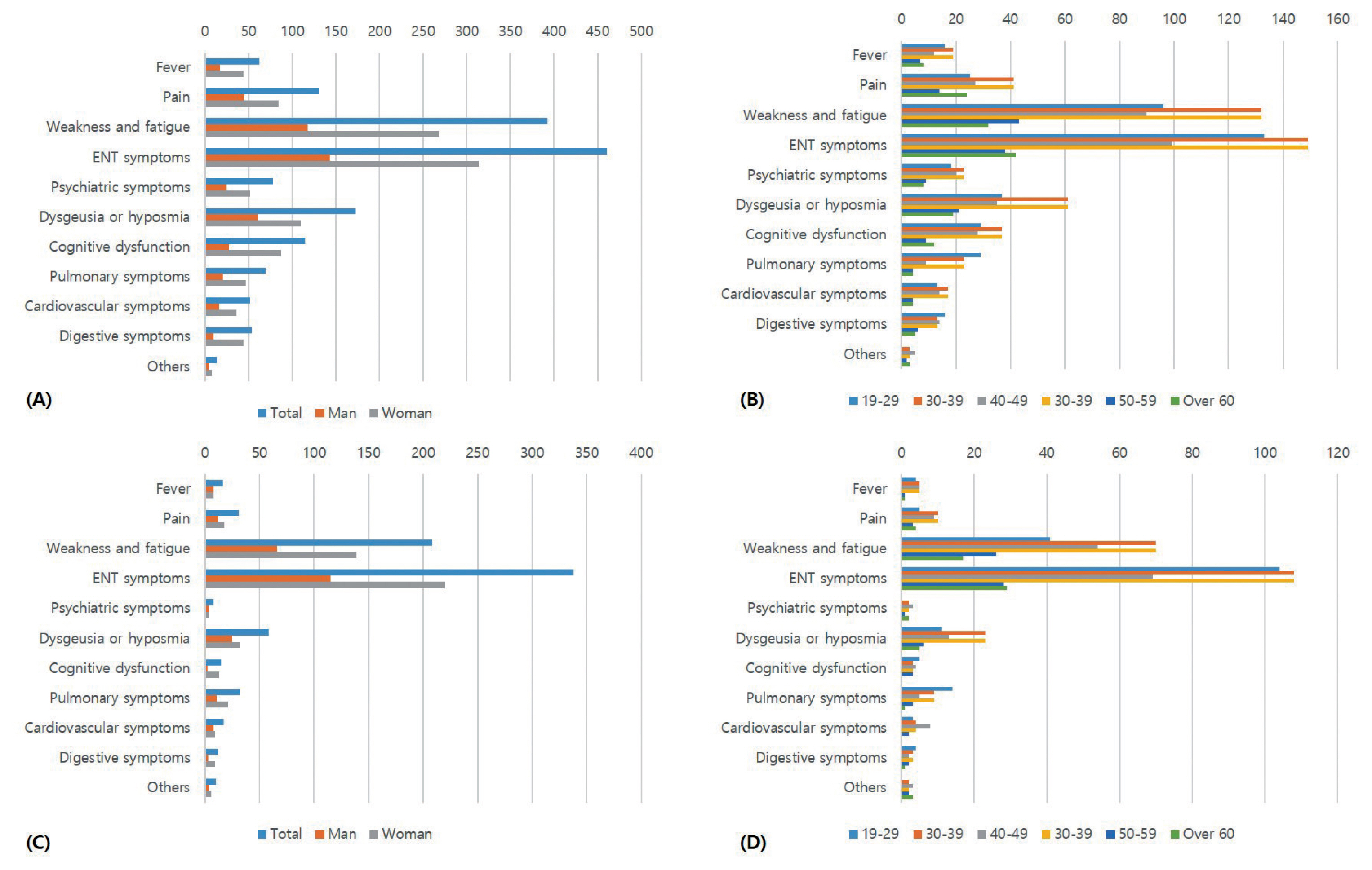
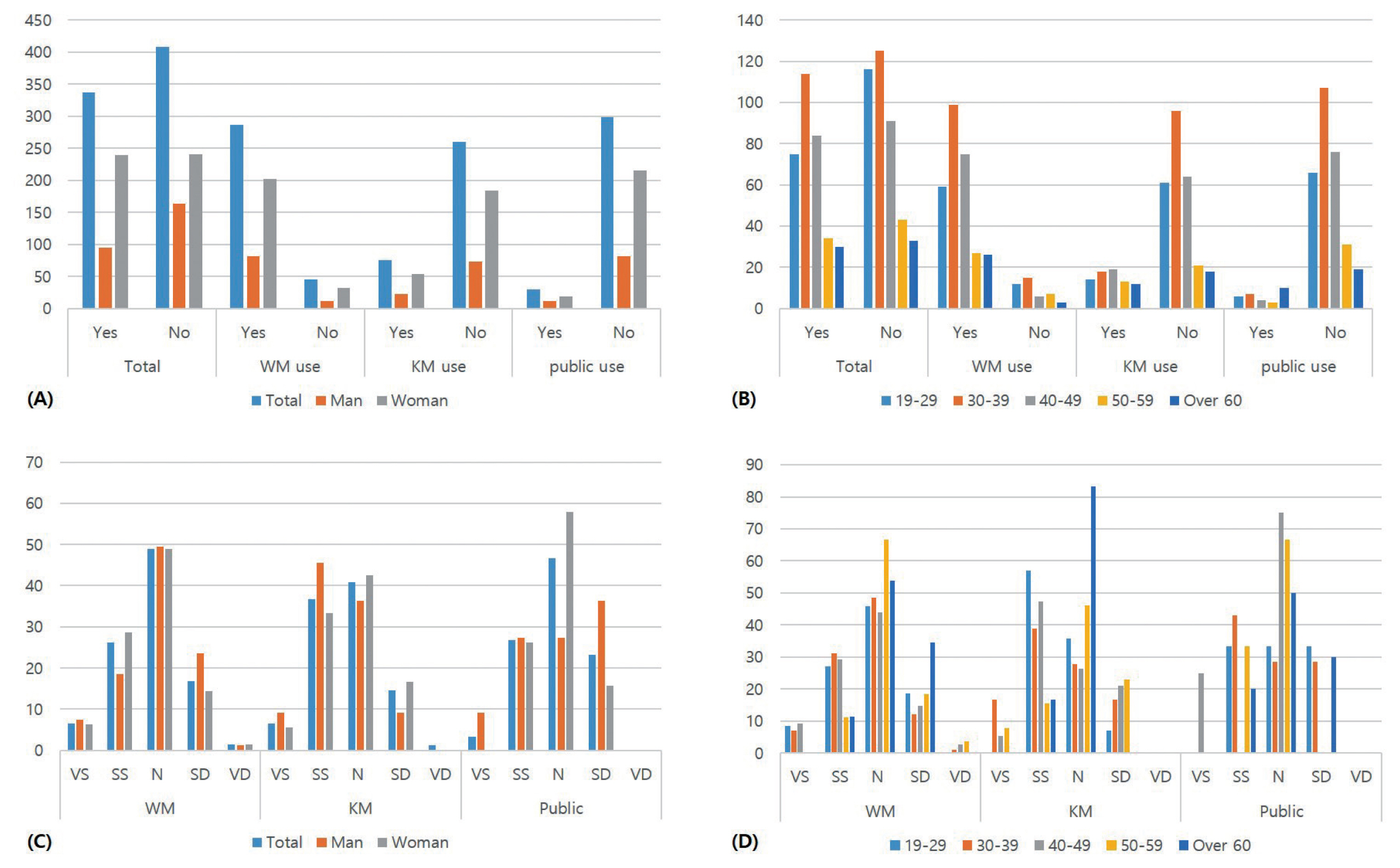
- 3. Medical access for long COVID
- Details and satisfaction with medical access long COVID are shown in Fig. 3 and Supplementary Table 2. The percentage of respondents with medical access was 45.2% (n = 337). The percentage of medical access was significantly higher amongst females (p < 0.0001) and lower in those respondents aged 19–29 years (p < 0.0001). Among respondents who had used medical institutions, 84.9% (n = 286) had used Western medicine (WM) clinics/hospitals, with the highest percentage receiving pharmaceutical therapy (n = 245, 85.7%). There were 76 respondents (22.6%) who used Korean medicine (KM) clinics/hospitals, with a higher percentage of use amongst respondents aged 50–59 years (38.2%) and 60–69 years (40%; p = 0.0086). The percentage of those who received herbal decoction was the highest, accounting for almost half of the treatments, followed by acupuncture and herbal powder. The percentages of respondents who were very satisfied/satisfied were 28,8%, 43.4%, and 40.0% for WM, KM, public institutions, respectively, showing the highest satisfaction with KM treatment.
- 4. Unmet medical needs and QoL of patients with long COVID
- Amongst the 745 long COVID patients, 242 (32.5%) indicated that they had unmet medical needs. Females and older patients tended to have a higher percentage of unmet medical needs. With respect to the reasons for unmet medical needs, difficulty in making time (20.1%) was the most common response, followed by insufficient information (10.3%), and burden of cost (7.1%; Fig. 4, Supplementary Table 2).
- The groups with unmet medical needs had a higher percent of comorbidities, moderate-severe symptoms, and severe symptoms (p < 0.0001). Duration of long COVID tended to be longer in the groups with unmet medical needs (p = 0.0002; Table 3).
- QoL was lower amongst those respondents who were female (p < 0.0001), older patients (p < 0.0001), living in capital areas other than Seoul (p = 0.0493), who had no occupation (p < 0.0001), with large household size (p = 0.0242), a lower level of education (p = 0.0056), comorbidities (p < 0.0001), higher severity of COVID-19 symptoms (p = 0.0034), higher severity of long COVID (p < 0.0001), longer duration of long COVID (p < 0.0001), and unmet medical needs (p < 0.0001; Table 3).
- 5. Need for long COVID support policies
- The responses regarding long COVID support policies are shown in Table 4. Amongst the 1,430 respondents, 760 respondents (53.1%) indicated that long COVID support policies were needed. The percentage of those who responded that such policies were needed was highest amongst females (p = 0.0025) and lowest amongst those aged 19–29 years (p < 0.0001).
- Preferred policies were the reduction of co-payment which was the most common response (n = 749, 52.4%), followed by health insurance coverage for non-covered items (n = 633, 44.3%), and information regarding care departments, and treatment methods by symptoms (n = 570, 39.9%). There were 913 respondents (63.8%) who indicated that they had the intention to use KM services, and this was highest amongst females and older patients (p = 0.0426; p = 0.0006).
- 6. Determinants of unmet medical needs
- The determinants of unmet medical needs are presented in Table 5. The univariate regression model analysis showed that the OR for unmet medical needs was higher among respondents who lived in capital areas other than Seoul (OR 1.53; 95% CI 1.05 to 2.23) and had comorbidities (OR 1.45; 95% CI 1.01 to 2.06). In addition, long COVID severity and a long duration of long COVID were identified as risk factors for unmet medical needs. The multivariate logistic model was established with the inclusion of all variables selected from the univariate model. The results showed that the area under the curve value was 0.710, and that living in capital areas other than Seoul, long COVID severity, and duration of long COVID were risk factors underlying unmet medical needs.
Results
- A web-based survey of 1,430 patients who experienced COVID-19 was conducted to investigate long COVID, medical access, and the need for long COVID support policies.
- Among 1,430 respondents, 545 (52.1%) experienced long COVID. Compared with the COVID-19 respondents who did not develop long COVID, the long COVID group showed a higher percentage of older respondents, a lower percentage of those without comorbidities and being asymptomatic during the acute phase of COVID-19, and a lower QoL. There have been various reports on the incidence of long COVID [12–16], and the findings in the present study did not significantly deviate from previous reports. Moreover, older age and severity of acute COVID-19 have been identified as risk factors for long COVID in previous studies [24,25,30]. The low QoL of post-COVID patients has also been reported [13, 20, 21], whereas low QoL in long COVID patients was associated with neuropsychiatric symptoms such as anxiety, sleep disturbance, and depression [25,26]. Particularly, the findings in the present study which showed a significant difference in EQ-5D scores according to experiencing long COVID, the severity of long COVID and their duration, indicating that long COVID have a major impact on QoL.
- The most common long COVID symptoms were ENT symptoms (n = 461, 61.9%), followed by weakness and fatigue (n = 393, 52.8%), and dysgeusia or hyposmia (n = 173, 23.2%). Almost half of the patients experienced mild to moderate severity of symptoms, meaning no significant impairment of day-to-day life but requiring treatment. Severity tended to be higher amongst females and older patients. The common duration of long COVID was 1–3 months (n = 329, 44.2%) and 2 weeks-1 month (n = 236, 31.7%). Many previous studies reported that the most common symptom of long COVID was fatigue [13,14,24,31], followed by dyspnea, dysgeusia, and hyposmia [10,12,13,15,16,23,31–33], which was different from the findings of the present study. Moreover, the percentage of respondents with ≥ 6 months of long COVID duration was approximately 2.3% in the present study, which was inconsistent with previous studies reporting that many patients experienced long COVID even at 6 and 12 months after infection [24–26]. Such differences could be explained by the fact that 75% of the respondents in the present study were patients who had developed COVID-19 in the last 100 days i.e., the later stages of the COVID-19 pandemic as opposed to the early stages of the pandemic.
- Amongst the 745 patients who experienced long COVID, 45.2% (n = 337) had used medical institutions. The respondents mostly accessed WM, but were more satisfied with KM treatment which included herbal decoctions (n = 39, 51.3%) and herbal powder (n = 24, 31.6%). Despite a significant amount of evidence on the effectiveness of oriental medicine in the acute phase of COVID-19 [34,35], and high satisfaction with KM among long COVID patients in the study, KM is not often used for treating long COVID, and relevant studies are very scarce. Studies on the effectiveness of KM were limited to a few cases [36,37]. Therefore, preclinical and clinical trials are needed to support the effectiveness of oriental medicine, such as herbal medicine and acupuncture, for long COVID.
- Meanwhile, 242 (32.5%) out of 745 long COVID patients indicated that they had unmet medical needs. The reasons for unmet medical needs included difficulty in finding time to visit medical care facilities (20.1%), insufficient information on long COVID care (10.3%), and burden of cost (7.1%). During a pandemic, there is a high likelihood of patients experiencing unmet medical needs due to avoidance and fear of crowded places and hospitals [27,28]; unmet medical needs have also increased due to the COVID-19 pandemic disrupting access to medical services [38]. Our findings determined that many patients with long COVID were experiencing unmet medical needs. Other reasons for unmet medical needs included “they would not see me because it was difficult to find an association with COVID-19” and “it was difficult to go to the hospital since the clinicians said that everyone has some long COVID and things will improve over time.”
- Unmet medical needs tended to be higher amongst females and older patients. Living in capital areas other than Seoul as well as long COVID severity and duration were risk factors for unmet medical needs. This suggested that people who must use medical services because of the high severity and long duration of symptoms did not receive appropriate treatment. Unmet medical needs also affected QoL, the group with unmet medical needs showed QoL scores that were 0.05 points lower than those with their medical needs met.
- Meanwhile, 760 respondents (53.1%) indicated that support policies for long COVID patients were needed. A reduction of co-payment was the most common suggestion for support policy (n = 749, 52.4%), followed by health insurance coverage (n = 633, 44.3%), and providing information (n = 570, 39.9%). This suggested that there was a significant need for financial support to use medical services. The responses above are also major reasons for unmet medical needs that could be considered in relation to burden of cost, and insufficient information. Accordingly, there is a need to establish policies related to appropriate treatment and recovery of QoL in patients with long COVID.
- Furthermore, 913 respondents (63.8%) indicated that they intend to use medical services if KM was covered by health insurance and policies, and programs for KM clinics were established. The intention to use KM treatment was high amongst females and older patients (p = 0.0426; p = 0.0006). As mentioned earlier, females and older patients have high unmet medical needs, suggesting that establishing policies related to KM treatment could effectively help meet their currently unmet medical needs.
- The present study was a web-based survey conducted through a mobile survey company and an announcement on the JMF website, and the respondents were limited to visitors to the JMF website and their acquaintances, and the registered panel of the survey company. However, the sample is believed to represent the entire Korean population because basic characteristics were evenly distributed. Another limitation of this study was that there is a possibility that the survey was conducted mainly on patients with mild symptoms, because the survey was conducted through an internet open survey. In fact, only 4.7% of the patients said the severity of COVID-19 symptoms were severe. However, since most patients have mild or moderate severity of COVID-19 symptoms, in reality, it was meaningful to examine patients with mild symptoms.
- This was the first study focusing on long COVID with a focus on the recent wave of COVID-19 in the first half of 2022. The study used a large-scale sample consisting of 1,360 individuals to comprehensively investigate the clinical features of long COVID, QoL, unmet medical needs, and the need for relevant COVID-19-related policies. Additional studies on the effectiveness of KM treatment for long COVID and policies to support appropriate treatment of long COVID patients are needed. The findings of this present study could be used as the basis for decision and policymaking by clinicians who treat long COVID patients, researchers, and COVID-19-related policymakers.
Discussion
Supplementary Materials
-
Author Contributions
Conceptualization: DK. Methodology: DK, and UMJ. Formal investigation: JYL. Data analysis: DK. Writing original draft: DK. Writing - review and editing: UMJ, and JYL.
-
Conflicts of Interest
The authors have no conflicts of interest to declare.
-
Funding
None.
-
Ethical Statement
This study referred to the Checklist for Reporting of Survey Studies, and the study protocol and questionnaire were approved by the Institutional Review Board of Jaseng Hospital of Korean Medicine (approval no.: JASENG 2022-05-005; approval date: 20 May 2022).
-
Data Availability
Raw data cannot be disclosed, and all relevant analyzed data are included in the manuscript and supplementary materials.
Article information
| Total | Long COVID | Non long COVID | p | |
|---|---|---|---|---|
| Total | 1,430 | 745 | 685 | |
| Sex | < 0.0001* | |||
| Man | 564 (39.4) | 258 (34.6) | 306 (44.7) | |
| Woman | 850 (59.4) | 479 (64.3) | 371 (54.2) | |
|
|
||||
| Age (y) | ||||
| mean ± SD | 38.20 ± 11.60 | 38.87 ± 11.36 | 37.42 ± 11.82 | 0.0192† |
| 19–29 | 397 (27.8) | 191 (25.6) | 206 (30.1) | 0.0037‡ |
| 30–39 | 488 (34.1) | 239 (32.1) | 249 (36.4) | |
| 40–49 | 285 (19.9) | 175 (23.5) | 110 (16.1) | |
| 50–59 | 136 (9.5) | 77 (10.3) | 59 (8.6) | |
| ≥ 60 | 124 (8.7) | 63 (8.5) | 61 (8.9) | |
|
|
||||
| Area of residence | 0.0554 | |||
| Seoul | 445 (31.1) | 229 (30.7) | 216 (31.5) | |
| Capital area other than Seoul | 446 (31.2) | 255 (34.2) | 191 (27.9) | |
| Metropolitan city | 312 (21.8) | 151 (20.3) | 161 (23.5) | |
| Others | 211 (14.8) | 102 (13.7) | 109 (15.9) | |
|
|
||||
| Occupation | 0.0519 | |||
| Manager | 146 (10.2) | 85 (11.4) | 61 (8.9) | |
| Professionals and related workers | 467 (32.7) | 230 (30.9) | 237 (34.6) | |
| Service workers | 219 (15.3) | 121 (16.2) | 98 (14.3) | |
| Sales workers | 27 (1.9) | 11 (1.5) | 16 (2.3) | |
| Skilled agricultural, forestry, and fishery workers | 6 (0.4) | 4 (0.5) | 2 (0.3) | |
| Craft and related trades workers | 31 (2.2) | 15 (2.0) | 16 (2.3) | |
| Equipment, machine operating and assembling workers | 14 (1.0) | 2 (0.3) | 12 (1.8) | |
| Elementary workers | 89 (6.2) | 51 (6.8) | 38 (5.5) | |
| Military personnel | 15 (1.0) | 5 (0.7) | 10 (1.5) | |
| No occupation (including homemakers and students) | 238 (16.6) | 129 (17.3) | 109 (15.9) | |
| Others | 162 (11.3) | 84 (11.3) | 78 (11.4) | |
|
|
||||
| Household size (members) | 0.8969 | |||
| 1 (live alone) | 261 (18.3) | 131 (17.6) | 130 (19.0) | |
| 2 | 274 (19.2) | 145 (19.5) | 129 (18.8) | |
| 3 | 367 (25.7) | 188 (25.2) | 179 (26.1) | |
| 4 | 433 (30.3) | 229 (30.7) | 204 (29.8) | |
| ≥ 5 | 79 (5.5) | 44 (5.9) | 35 (5.1) | |
|
|
||||
| Household income (won) | 0.4799 | |||
| < 2,000,000 | 88 (6.2) | 39 (5.2) | 49 (7.2) | |
| 2,000,000–4,999,999 | 667 (46.6) | 342 (45.9) | 325 (47.4) | |
| 5,000,000–7,999,999 | 389 (27.2) | 211 (28.3) | 178 (26.0) | |
| 8,000,000–9,999,999 | 141 (9.9) | 74 (9.9) | 67 (9.8) | |
| ≥ 10,000,000 | 129 (9.0) | 71 (9.5) | 58 (8.5) | |
|
|
||||
| Education level | 0.5418 | |||
| College or higher | 1,195 (83.6) | 627 (84.2) | 568 (82.9) | |
| High school or below | 219 (15.3) | 110 (14.8) | 109 (15.9) | |
| Comorbidities | ||||
| None | 1,129 (79.0) | 565 (75.8) | 564 (82.3) | 0.0026‡ |
| Hypertension | 127 (8.9) | 66 (8.9) | 61 (8.9) | 0.9756 |
| Diabetes | 57 (4.0) | 33 (4.4) | 24 (3.5) | 0.3713 |
| Cardiovascular disease | 20 (1.4) | 9 (1.2) | 11 (1.6) | 0.5222 |
| Cerebrovascular disease | 6 (0.4) | 6 (0.8) | 0 (0.0) | 0.0317† |
| Respiratory disease | 25 (1.7) | 19 (2.6) | 6 (0.9) | 0.0158† |
| Cancer | 23 (1.6) | 14 (1.9) | 9 (1.3) | 0.3959 |
| Mental illness | 24 (1.7) | 18 (2.4) | 6 (0.9) | 0.0235† |
| Others | 62 (4.3) | 38 (5.1) | 24 (3.5) | 0.1385 |
|
|
||||
| Days after COVID-19 diagnosis | ||||
| Mean ± SD | 98.90 ± 77.60 | 97.56 ± 73.59 | 100.34 ± 81.86 | 0.5013 |
| Median (Q1, Q3) | 86 (70, 101) | 87 (70, 100) | 86 (69, 102) | |
|
|
||||
| Symptoms of COVID-19 | ||||
| Asymptomatic | 35 (2.4) | 7 (0.9) | 28 (4.1) | 0.0001* |
| Fever | 876 (61.3) | 491 (65.9) | 385 (56.2) | 0.0002* |
| Pain | 730 (51.0) | 444 (59.6) | 286 (41.8) | < 0.0001* |
| Weakness and fatigue | 852 (59.6) | 501 (67.2) | 351 (51.2) | < 0.0001* |
| ENT symptoms | 1,201 (84.0) | 662 (88.9) | 539 (78.7) | < 0.0001* |
| Psychiatric symptoms | 120 (8.4) | 92 (12.3) | 28 (4.1) | < 0.0001* |
| Dysgeusia or hyposmia | 381 (26.6) | 261 (35.0) | 120 (17.5) | < 0.0001* |
| Pulmonary symptoms | 156 (10.9) | 129 (17.3) | 27 (3.9) | < 0.0001* |
| Cardiovascular symptoms | 67 (4.7) | 53 (7.1) | 14 (2.0) | < 0.0001* |
| Digestive symptoms | 200 (14.0) | 142 (19.1) | 58 (8.5) | < 0.0001* |
| Others | 28 (2.0) | 19 (2.6) | 9 (1.3) | 0.0918 |
|
|
||||
| Severity of acute COVID-19 | < 0.0001* | |||
| Asymptomatic | 89 (6.2) | 26 (3.5) | 63 (9.2) | |
| Mild | 1,321 (92.4) | 706 (94.8) | 615 (89.8) | |
| Moderate | 19 (1.3) | 13 (1.7) | 6 (0.9) | |
| Severe | 1 (0.1) | 1 (0.1) | ||
| EQ-5D (mean ± SD) | 0.94 ± 0.10 | 0.92 ± 0.11 | 0.97 ± 0.06 | < 0.0001* |
| Total | Total | Sex | Age (y) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||
| Male | Female | p | 19–29 | 30–39 | 40–49 | 50–59 | ≥ 60 | p | ||
| 745 | 258 | 479 | 191 | 239 | 175 | 77 | 63 | |||
| Overall severity | 0.0030* | 0.0092* | ||||||||
| Mild | 183 (24.6) | 80 (31.0) | 101 (21.1) | 40 (20.9) | 59 (24.7) | 39 (22.3) | 30 (39.0) | 15 (23.8) | ||
| Mild to moderate | 357 (47.9) | 121 (46.9) | 233 (48.6) | 96 (50.3) | 122 (51.0) | 81 (46.3) | 35 (45.5) | 23 (36.5) | ||
| Moderate to severe | 170 (22.8) | 43 (16.7) | 125 (26.1) | 51 (26.7) | 47 (19.7) | 45 (25.7) | 8 (10.4) | 19 (30.2) | ||
| Severe | 35 (4.7) | 14 (5.4) | 20 (4.2) | 4 (2.1) | 11 (4.6) | 10 (5.7) | 4 (5.2) | 6 (9.5) | ||
|
|
||||||||||
| Onset of symptoms | 0.0645 | 0.3558 | ||||||||
| Continued from diagnosed | 453 (60.8) | 140 (54.3) | 310 (64.7) | 126 (66.0) | 144 (60.3) | 102 (58.3) | 44 (57.1) | 37 (58.7) | ||
| Within 2 wks | 139 (18.7) | 52 (20.2) | 84 (17.5) | 37 (19.4) | 43 (18.0) | 38 (21.7) | 10 (13.0) | 11 (17.5) | ||
| 2 wks-1 mo | 98 (13.2) | 42 (16.3) | 55 (11.5) | 19 (9.9) | 36 (15.1) | 21 (12.0) | 14 (18.2) | 8 (12.7) | ||
| 1–3 mo | 47 (6.3) | 21 (8.1) | 25 (5.2) | 7 (3.7) | 16 (6.7) | 12 (6.9) | 6 (7.8) | 6 (9.5) | ||
| Over 3 mo | 8 (1.1) | 3 (1.2) | 5 (1.0) | 2 (1.0) | 2 (1.1) | 3 (3.9) | 1 (1.6) | |||
|
|
||||||||||
| Duration of long COVID | 0.8420 | 0.2471 | ||||||||
| Under 2 wks | 73 (9.8) | 27 (10.5) | 46 (9.6) | 20 (10.5) | 20 (8.4) | 19 (10.9) | 10 (13.0) | 4 (6.3) | ||
| 2 wks-1 mo | 236 (31.7) | 78 (30.2) | 154 (32.2) | 68 (35.6) | 79 (33.1) | 56 (32.0) | 19 (24.7) | 14 (22.2) | ||
| 1–3 mo | 329 (44.2) | 111 (43.0) | 214 (44.7) | 77 (40.3) | 115 (48.1) | 73 (41.7) | 34 (44.2) | 30 (47.6) | ||
| 3–6 mo | 90 (12.1) | 36 (14.0) | 54 (11.3) | 21 (11.0) | 23 (9.6) | 22 (12.6) | 11 (14.3) | 13 (20.6) | ||
| Over 6 mo | 17 (2.3) | 6 (2.3) | 11 (2.3) | 5 (2.6) | 2 (0.8) | 5 (2.9) | 3 (3.9) | 2 (3.2) | ||
| Total | Unmet medical needs | QoL | p | ||
|---|---|---|---|---|---|
|
|
|||||
| Yes | No | p | |||
|
|
|
||||
| 242 | 503 | 745 | |||
| Sex | |||||
| Man | 77 (31.8) | 181 (36.0) | 0.2476 | 0.96 ± 0.09 | < 0.0001* |
| Woman | 163 (67.4) | 316 (62.8) | 0.93 ± 0.10 | ||
|
|
|||||
| Age (y) | |||||
| 19–29 | 54 (22.3) | 137 (27.2) | 0.6518 | 0.96 ± 0.08 | < 0.0001* |
| 30–39 | 81 (33.5) | 158 (31.4) | 0.95 ± 0.10 | ||
| 40–49 | 57 (23.6) | 118 (23.5) | 0.93 ± 0.09 | ||
| 50–59 | 27 (11.2) | 50 (9.9) | 0.92 ± 0.11 | ||
| ≥ 60 | 23 (9.5) | 40 (8.0) | 0.92 ± 0.12 | ||
|
|
|||||
| Area of residence | |||||
| Seoul | 68 (28.1) | 161 (32.0) | 0.0458† | 0.95 ± 0.09 | 0.0493† |
| Capital area other than Seoul | 100 (41.3) | 155 (30.8) | 0.93 ± 0.10 | ||
| Five major metropolitan cities | 42 (17.4) | 109 (21.7) | 0.95 ± 0.10 | ||
| Others | 30 (12.4) | 72 (14.3) | 0.95 ± 0.08 | ||
|
|
|||||
| Occupation | |||||
| Yes | 408 (81.1) | 200 (82.6) | 0.6779 | 0.95 ± 0.09 | < 0.0001* |
| No | 89 (17.7) | 40 (16.5) | 0.92 ± 0.12 | ||
|
|
|||||
| Household size | |||||
| 1 (live alone) | 82 (16.3) | 49 (20.2) | 0.4743 | 0.96 ± 0.08 | 0.0242† |
| 2 | 93 (18.5) | 52 (21.5) | 0.95 ± 0.09 | ||
| 3 | 131 (26.0) | 57 (23.6) | 0.94 ± 0.10 | ||
| 4 | 159 (31.6) | 70 (28.9) | 0.94 ± 0.10 | ||
| ≥ 5 | 32 (6.4) | 12 (5.0) | 0.93 ± 0.10 | ||
|
|
|||||
| Household income (won) | |||||
| < 2,000,000 | 16 (6.6) | 23 (4.6) | 0.4836 | 0.94 ± 0.10 | 0.7629 |
| 2,000,000–4,999,999 | 112 (46.3) | 230 (45.7) | 0.94 ± 0.09 | ||
| 5,000,000–7,999,999 | 72 (29.8) | 139 (27.6) | 0.94 ± 0.10 | ||
| 8,000,000–9,999,999 | 22 (9.1) | 52 (10.3) | 0.94 ± 0.11 | ||
| ≥ 10,000,000 | 18 (7.4) | 53 (10.5) | 0.95 ± 0.08 | ||
|
|
|||||
| Education level | |||||
| College or higher | 200 (82.6) | 427 (84.9) | 0.3566 | 0.95 ± 0.09 | 0.0055‡ |
| High school or below | 40 (16.5) | 70 (13.9) | 0.92 ± 0.12 | ||
|
|
|||||
| Comorbidities | |||||
| No | 173 (71.5) | 392 (77.9) | 0.0411† | 0.95 ± 0.08 | < 0.0001‡ |
| Yes | 67 (27.7) | 105 (20.9) | 0.90 ± 0.13 | ||
|
|
|||||
| Severity of COVID-19 | |||||
| Asymptomatic | 6 (2.5) | 20 (4.0) | 0.3397 | 0.96 ± 0.10 | 0.0034‡ |
| Mild | 230 (95.0) | 476 (94.6) | 0.94 ± 0.09 | ||
| Moderate | 6 (2.5) | 7 (1.4) | 0.88 ± 0.18 | ||
| Severe | 0.87 ± . | ||||
|
|
|||||
| Severity of long COVID | |||||
| Mild | 32 (13.2) | 151 (30.0) | < 0.0001* | 0.95 ± 0.10 | < 0.0001* |
| Mild-moderate | 127 (52.5) | 230 (45.7) | 0.91 ± 0.10 | ||
| Moderate-severe | 69 (28.5) | 101 (20.1) | 0.92 ± 0.10 | ||
| Severe | 14 (5.8) | 21 (4.2) | 0.80 ± 0.17 | ||
|
|
|||||
| Duration of long COVID | |||||
| Under 2 wks | 15 (6.2) | 58 (11.5) | 0.0002* | 0.93 ± 0.13 | < 0.0001* |
| 2 wks-1 mo | 57 (23.6) | 179 (35.6) | 0.94 ± 0.08 | ||
| 1–3 mo | 129 (53.3) | 200 (39.8) | 0.91 ± 0.11 | ||
| 3–6 mo | 32 (13.2) | 58 (11.5) | 0.85 ± 0.14 | ||
| Over 6 mo | 9 (3.7) | 8 (1.6) | 0.88 ± 0.10 | ||
|
|
|||||
| Unmet medical needs | |||||
| Yes | 0.88 ± 0.13 | < 0.0001 | |||
| No | 0.93 ± 0.10 | ||||
Unmet medical needs are presented as frequency (%), and QoL is presented as mean ± SD. The p-value of unmet medical needs was calculated using the chi-square test or Fisher’s exact test, while the p value of QoL was calculated using an independent t-test or ANOVA.
* p < 0.001,
† p < 0.5,
‡ p < 0.01.
| Total (N) | Total | Sex | Age | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||
| Male | Female | p | 19–29 | 30–39 | 40–49 | 50–59 | ≥ 60 | p | ||
| 1,430 | 564 | 850 | 397 | 488 | 285 | 136 | 124 | |||
| Need for long COVID support policies | ||||||||||
| Yes | 760 (53.1) | 284 (50.4) | 470 (55.3) | 0.0025* | 178 (44.8) | 275 (56.4) | 169 (59.3) | 68 (50.0) | 70 (56.5) | < 0.0001† |
| No | 326 (22.8) | 156 (27.7) | 168 (19.8) | 83 (20.9) | 114 (23.4) | 53 (18.6) | 45 (33.1) | 31 (25.0) | ||
| Not sure | 336 (23.5) | 124 (22.0) | 212 (24.9) | 128 (32.2) | 99 (20.3) | 63 (22.1) | 23 (16.9) | 23 (18.5) | ||
|
|
||||||||||
| Preferred and necessary policies | ||||||||||
| Reduction of co-payment | 749 (52.4) | 317 (56.2) | 427 (50.2) | 0.0277‡ | 225 (56.7) | 262 (53.7) | 155 (54.4) | 55 (40.4) | 52 (41.9) | 0.0020* |
| Expansion of health insurance | 633 (44.3) | 265 (47.0) | 364 (42.8) | 0.1230 | 181 (45.6) | 202 (41.4) | 138 (48.4) | 59 (43.4) | 53 (42.7) | 0.3967 |
| Information availability | 570 (39.9) | 214 (37.9) | 355 (41.8) | 0.1513 | 142 (35.8) | 205 (42.0) | 104 (36.5) | 60 (44.1) | 59 (47.6) | 0.0569 |
| Establishment of counseling clinics | 211 (14.8) | 68 (12.1) | 141 (16.6) | 0.0187‡ | 44 (11.1) | 80 (16.4) | 45 (15.8) | 29 (21.3) | 13 (10.5) | 0.0173‡ |
| Establishment of specialized treatment clinics | 266 (18.6) | 101 (17.9) | 161 (18.9) | 0.6243 | 69 (17.4) | 97 (19.9) | 51 (17.9) | 25 (18.4) | 24 (19.4) | 0.9005 |
| Others (fill in) | 18 (1.3) | 18 (3.2) | 0 (0.0) | 6 (1.5) | 0 (0.0) | 6 (2.1) | 0 (0.0) | 6 (4.8) | ||
|
|
||||||||||
| Intention to use KM service | ||||||||||
| Yes | 913 (63.8) | 348 (61.7) | 558 (65.6) | 0.0426‡ | 223 (56.2) | 308 (63.1) | 200 (70.2) | 90 (66.2) | 92 (74.2) | 0.0006† |
| No | 288 (20.1) | 133 (23.6) | 154 (18.1) | 83 (20.9) | 116 (23.8) | 44 (15.4) | 28 (20.6) | 17 (13.7) | ||
| Not sure | 221 (15.5) | 83 (14.7) | 138 (16.2) | 83 (20.9) | 64 (13.1) | 41 (14.4) | 18 (13.2) | 15 (12.1) | ||
| Univariate model | Multivariate model | |
|---|---|---|
| Sex (Ref=male) | ||
| Female | 1.21 (0.87 – 1.68) | 1.13 (0.78 – 1.63) |
| Age in years (Ref=19–29) | ||
| 30–39 | 1.30 (0.86 – 1.97) | 1.37 (0.85 – 2.21) |
| 40–49 | 1.23 (0.78 – 1.91) | 1.22 (0.73 – 2.04) |
| 50–59 | 1.37 (0.78 – 2.41) | 1.61 (0.84 – 3.09) |
| ≥ 60 | 1.46 (0.80 – 2.66) | 1.29 (0.62 – 2.70) |
|
|
||
| Area of residence (Ref=Seoul) | ||
| Capital area other than Seoul | 1.53 (1.05 – 2.23)* | 1.69 (1.11 – 2.59)* |
| Five major metropolitan cities | 0.91 (0.58 – 1.44) | 1.01 (0.61 – 1.66) |
| Others | 0.99 (0.59– 1.65) | 1.31 (0.74 – 2.32) |
| Occupation (Ref=no) | ||
| Yes | 1.09 (0.72 – 1.64) | 1.11 (0.69 – 1.80) |
|
|
||
| Household size (Ref=1) | ||
| 2 | 0.94 (0.57 – 1.53) | 0.77 (0.44 – 1.36) |
| 3 | 0.73 (0.45 – 1.17) | 0.60 (0.34 – 1.06) |
| 4 | 0.74 (0.47 – 1.16) | 0.69 (0.40 – 1.22) |
| ≥ 5 | 0.63 (0.30 – 1.33) | 0.45 (0.19 – 1.07) |
|
|
||
| Household income (Ref=< 2,000,000) | ||
| 2,000,000–4,999,999 | 0.70 (0.36 – 1.38) | 0.65 (0.30 – 1.41) |
| 5,000,000–7,999,999 | 0.74 (0.37 – 1.50) | 0.70 (0.31 – 1.58) |
| 8,000,000–9,999,999 | 0.61 (0.27 – 1.37) | 0.53 (0.20 – 1.38) |
| ≥ 10,000,000 | 0.49 (0.21 – 1.12) | 0.47 (0.18 – 1.25) |
|
|
||
| Education level (Ref= college or higher) | ||
| High school or below | 1.22 (0.80 – 1.86) | 1.14 (0.69 – 1.88) |
| Comorbidities (Ref=no) | ||
| Yes | 1.45 (1.01 – 2.06)* | 1.22 (0.80 – 1.86) |
| Severity of COVID-19 (Ref=asymptomatic) | ||
| Mild | 1.61 (0.64 – 4.06) | 1.22 (0.45 – 3.31) |
| Moderate | 2.86 (0.69 – 11.83) | 1.64 (0.35 – 7.71) |
| Severe | ||
|
|
||
| Overall severity of long COVID (Ref=mild) | ||
| Mild-moderate | 2.61 (1.68 – 4.04)† | 2.35 (1.46 – 3.76)† |
| Moderate-severe | 3.22 (1.98 – 5.26)† | 3.13 (1.83 – 5.36)† |
| Severe | 3.15 (1.45 – 6.84)‡ | 1.83 (0.74 – 4.54) |
|
|
||
| Duration of long COVID (Ref= < 2 wks) | ||
| 2 wks-1 mo | 1.23 (0.65 – 2.34) | 1.13 (0.56 – 2.26) |
| 1–3 mo | 2.49 (1.36 – 4.59)‡ | 2.32 (1.20 – 4.50)* |
| 3–6 mo | 2.13 (1.05 – 4.35)* | 1.90 (0.87 – 4.15) |
| Over 6 mo | 4.35 (1.44 – 13.18)† | 3.84 (1.16 – 12.76)* |
| AUC | 0.71 | |
- [1] Guo YR, Cao QD, Hong ZS, Tan YY, Chen SD, Jin HJ, et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak-an update on the status. Mil Med Res 2020;7(1):11. ArticlePubMedPMCPDF
- [2] World Health Organization [Internet]. WHO Coronavirus (COVID-19) Dashboard: [cited 2022 Jun 27]. Available from: https://covid19.who.int/
- [3] Alimohamadi Y, Sepandi M, Taghdir M, Hosamirudsari H. Determine the most common clinical symptoms in COVID-19 patients: a systematic review and meta-analysis. J Prev Med Hyg 2020;61(3):E304−12.ArticlePubMedPMC
- [4] Al-Aly Z, Xie Y, Bowe B. High-dimensional characterization of post-acute sequelae of COVID-19. Nature 2021;594(7862):259−64.ArticlePubMedPDF
- [5] Krishnan A, Hamilton JP, Alqahtani SA, Woreta TA. COVID-19: An overview and a clinical update. World J Clin Case 2021;9(1):8−23.Article
- [6] Stokes EK, Zambrano LD, Anderson KN, Marder EP, Raz KM, El Burai Felix S, et al. Coronavirus Disease 2019 Case Surveillance - United States, January 22–May 30, 2020. MMWR Morb Mortal Wkly Rep 2020;69(24):759−65.ArticlePubMedPMC
- [7] Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, et al. Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern Med 2020;180(7):934−43.ArticlePubMed
- [8] National Institutes of Health [Internet]. COVID-19 Treatment Guidelines: [cited 2022 Jun 28]. Available from: https://www.covid19treatmentguidelines.nih.gov/
- [9] Tsui TK, Li CH, Poon KH, Lam DSY. Acupuncture Induced Bilateral Pneumothorax in Children Hong Kong. J Paediatr 2017;22(3):163−6.
- [10] Aiyegbusi OL, Hughes SE, Turner G, Rivera SC, McMullan C, Chandan JS, et al. Symptoms, complications and management of long COVID: a review. J R Soc Med 2021;114(9):428−42.ArticlePubMedPMCPDF
- [11] Centers for Disease Control and Prevention [Internet]. Long COVID or Post-COVID conditions: [cited 2022 Jun 28]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html
- [12] Logue JK, Franko NM, McCulloch DJ, McDonald D, Magedson A, Wolf CR, et al. Sequelae in Adults at 6 Months After COVID-19 Infection. JAMA Netw Open 2021;4(2):e210830. ArticlePubMedPMC
- [13] Carfì A, Bernabei R, Landi F. Persistent Symptoms in Patients After Acute COVID-19. JAMA 2020;324(6):603−5.ArticlePubMedPMC
- [14] Huang C, Huang L, Wang Y, Li X, Ren L, Gu X, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet 2021;397(10270):220−32.ArticlePubMedPMC
- [15] Chopra V, Flanders SA, O’Malley M, Malani AN, Prescott HC. Sixty-Day Outcomes Among Patients Hospitalized With COVID-19. Ann Intern Med 2021;174(4):576−8.ArticlePubMed
- [16] Carvalho-Schneider C, Laurent E, Lemaignen A, Beaufils E, Bourbao-Tournois C, Laribi S, et al. Follow-up of adults with noncritical COVID-19 two months after symptom onset. Clin Microbiol Infect 2021;27(2):258−63.ArticlePubMed
- [17] Gupta A, Madhavan MV, Sehgal K, Nair N, Mahajan S, Sehrawat TS, et al. Extrapulmonary manifestations of COVID-19. Nat Med 2020;26(7):1017−32.ArticlePubMedPDF
- [18] Nalbandian A, Sehgal K, Gupta A, Madhavan MV, McGroder C, Stevens JS, et al. Post-acute COVID-19 syndrome. Nature Med 2021;27(4):601−15.ArticlePubMedPDF
- [19] Cabrera Martimbianco AL, Pacheco RL, Bagattini ÂM, Riera R. Frequency, signs and symptoms, and criteria adopted for long COVID-19: A systematic review. Int J Clin Pract 2021;75(10):e14357. ArticlePubMedPDF
- [20] Iqbal A, Iqbal K, Arshad Ali S, Azim D, Farid E, Baig MD, et al. The COVID-19 Sequelae: A Cross-Sectional Evaluation of Post-recovery Symptoms and the Need for Rehabilitation of COVID-19 Survivors. Cureus 2021;13(2):e13080. ArticlePubMedPMC
- [21] Daher A, Balfanz P, Cornelissen C, Müller A, Bergs I, Marx N, et al. 2019 (COVID-19): Pulmonary and extrapulmonary disease sequelae. Respir Med 2020;174:106197. PubMedPMC
- [22] Frontera JA, Yang D, Lewis A, Patel P, Medicherla C, Arena V, et al. A prospective study of long-term outcomes among hospitalized COVID-19 patients with and without neurological complications. J Neurol Sci 2021;426:117486. ArticlePubMedPMC
- [23] Tabacof L, Tosto-Mancuso J, Wood J, Cortes M, Kontorovich A, McCarthy D, et al. Post-acute COVID-19 Syndrome Negatively Impacts Physical Function, Cognitive Function, Health-Related Quality of Life, and Participation. Am J Phys Med Rehabil 2022;101(1):48−52.ArticlePubMed
- [24] Kim Y, Kim S-W, Chang H-H, Kwon KT, Bae S, Hwang S. Significance and associated factors of long-term sequelae in patients after acute COVID-19 infection in Korea. Infect Chemother 2021;53(3):463−76.ArticlePubMedPMCPDF
- [25] Kim Y, Bitna H, Kim SW, Chang HH, Kwon KT, Bae S, et al. Post-acute COVID-19 syndrome in patients after 12 months from COVID-19 infection in Korea. BMC Infect Dis 2022;22(1):93. ArticlePubMedPMCPDF
- [26] Kim Y, Kim SW, Chang HH, Kwon KT, Hwang S, Bae S. One Year Follow-Up of COVID-19 Related Symptoms and Patient Quality of Life: A Prospective Cohort Study. Yonsei Med J 2022;63(6):499−510.ArticlePubMedPMCPDF
- [27] Kim J, You M, Shon C. Impact of the COVID-19 pandemic on unmet healthcare needs in Seoul, South Korea: A cross-sectional study. BMJ Open 2021;11(8):e045845. ArticlePubMed
- [28] Ahn S, Kim S, Koh K. [Internet]. Changes in healthcare utilization, spending, and perceived health during COVID-19: A longitudinal study from Singapore. Spending, and Perceived Health during COVID-19: A Longitudinal Study from Singapore: 2020 September Available from: https://www.iza.org/publications/dp/13715/changes-in-healthcare-utilization-spending-and-perceived-health-during-covid19-a-longitudinal-study-from-singapore
- [29] Pinato DJ, Tabernero J, Bower M, Scotti L, Patel M, Colomba E, et al. Prevalence and impact of COVID-19 sequelae on treatment and survival of patients with cancer who recovered from SARS-CoV-2 infection: evidence from the OnCovid retrospective, multicentre registry study. Lancet Oncol 2021;22(12):1669−80.PubMedPMC
- [30] Boscolo-Rizzo P, Guida F, Polesel J, Marcuzzo AV, Capriotti V, D’Alessandro A, et al. Sequelae in adults at 12 months after mild-to-moderate coronavirus disease 2019 (COVID-19). Int Forum Allergy Rhinol 2021;11(12):1685−8.ArticlePubMedPMCPDF
- [31] Arnold DT, Hamilton FW, Milne A, Morley AJ, Viner J, Attwood M, et al. Patient outcomes after hospitalisation with COVID-19 and implications for follow-up: results from a prospective UK cohort. Thorax 2021;76(4):399−401.ArticlePubMed
- [32] Halpin SJ, McIvor C, Whyatt G, Adams A, Harvey O, McLean L, et al. Postdischarge symptoms and rehabilitation needs in survivors of COVID-19 infection: a cross-sectional evaluation. Med Virol 2021;93(2):1013−22.ArticlePDF
- [33] Moreno-Pérez O, Merino E, Leon-Ramirez J-M, Andres M, Ramos JM, Arenas-Jiménez J, et al. Post-acute COVID-19 syndrome. Incidence and risk factors: A Mediterranean cohort study. J Infect 2021;82(3):378−83.ArticlePubMedPMC
- [34] Hu K, Guan W-j, Bi Y, Zhang W, Li L, Zhang B, et al. Efficacy and safety of Lianhuaqingwen capsules, a repurposed Chinese herb, in patients with coronavirus disease 2019: a multicenter, prospective, randomized controlled trial. Phytomedcine 2021;85:153242. Article
- [35] Zhou S, Feng J, Xie Q, Huang T, Xu X, Zhou D, et al. Traditional Chinese medicine shenhuang granule in patients with severe/critical COVID-19: A randomized controlled multicenter trial. Phytomedicine 2021;89:153612. ArticlePubMedPMC
- [36] Jania C. The Treatment of Long COVID with Chinese Medicine: A Case Report. J Chin Med 2021;127:17−22.
- [37] Trager RJ, Brewka EC, Kaiser CM, Patterson AJ, Dusek JA. Acupuncture in Multidisciplinary Treatment for Post-COVID-19 Syndrome. Med Acupunct 2022;34(3):177−83.ArticlePubMedPMC
- [38] World Health Organization [Internet]. COVID-19 continues to disrupt essential health services in 90% of countries: 2021 [cited 2022 Jul 25]. Available from: https://www.who.int/news/item/23-04-2021-covid-19-continues-to-disrupt-essential-health-services-in-90-of-countries


 PubReader
PubReader ePub Link
ePub Link Cite
Cite